Introduction
Injecting drug use is associated with significant health harms and risks such as HIV and HCV. Eight persons who inject drugs (PWID) live with HIV, and half of all PWID live with HCV. HCV is the leading cause of death in this population, particularly among those co-infected with HIV (Ly et al., 2012).
In Mexico, 1.3% of the population aged 12-65 years old has injected at least once an illegal substance (Villatoro-Velázquez et al., 2017). The Northern cities of Ciudad Juárez (state of Chihuahua), Tijuana (state of Baja California), and Hermosillo (state of Sonora) are home to the largest population of PWID in the country, representing an estimated 44% of the total Mexican population of PWID (N = 53,284) (Censida, 2010).
Although there is extensive literature on drug use trajectories and transition to injection among people who use drug users worldwide (Ambekar et al., 2019; Baluku, Wamala, & Muhangi, 2019; Bluthenthal, Wenger, Chu, Bourgois, & Kral, 2017; Brecht, Huang, Evans, & Hser, 2008; Horyniak et al., 2015; Hser, 2007; Koozegar, Shahesmaeili, & Noroozi, 2018; Neaigus et al., 2001; Oliveira et al., 2006; Roy et al., 2003; Vidal-Trecan, Varescon-Pousson, & Boissonnas, 2002), in Mexico, the literature is still limited and, in most cases, restricted to PWID who live in Tijuana (Bloom et al., 2021; Fuller et al., 2002; Ben Hamida et al., 2018; Meyers et al., 2021; Mittal et al., 2019; Morris et al., 2012; Rafful et al., 2018; Robertson, Lozada, Pollini, Rangel, & Ojeda, 2012).
In a recent work, Fleiz-Bautista et al. (2019) describe and compare the dynamics of drug use and risk practices for HIV and VHC, as well as HIV and VHC prevalence among PWID from Tijuana, Ciudad Juárez and San Luis Río Colorado, Sonora. Even though the crucial insights about the differential risk environments in these cities, mainly the information gathered for Sonora, the study does not intend to describe drug use trajectories.
The information about PWID dynamics is scarce for Sonora and Hermosillo. The latter is a city located at 178 miles from Tucson, AZ, where epidemiologic surveillance suggests an increasing prevalence of HIV infection and injection drug use (Ospina-Escobar et al., 2018). Currently, Hermosillo is the third city with the highest volume of PWID (Censida, 2010), among which the HIV prevalence is estimated at 5.2% (Bautista, Colchero, Sosa, & Conde, 2012).
The rapid expansion of HIV and injection drug use in Hermosillo could be associated, among other factors, with the dynamics of transition to injecting and the interval between the initiation of illicit drug use and the onset of drug injection. Shorter interval is accompanied by more prolonged exposure to high-risk behaviors (Abelson et al., 2006; Doherty, Garfein, Monterroso, Brown, & Vlahov, 2000; Garfein, Vlahov, Galai, Doherty, & Nelson, 1996; Vorobjov et al., 2013). Literature also shows that the period of transition into injecting has been characterized by an increased incidence of blood-borne disease transmission through the sharing of contaminated syringes, unplanned events, reliance on third-party assistance, and the sharing of injecting equipment (Crofts, Louie, Rosenthal, & Jolley, 1996; Fuller et al., 2002; Koozegar et al., 2018; Neaigus et al., 2001; Oliveira et al., 2006; Vidal-Trecan et al., 2002).
Given the relatively new syndemic of injecting drugs and HIV in Hermosillo, in this paper we compare the characteristics of the transition to injecting reported by PWID in this city with those reported by PWID from Ciudad Juárez, a city with an old history of drug injecting population. Ciudad Juárez is located at the midpoint of the 2,000 miles long border between Mexico and the United States, and is part of a metroplex with El Paso, Texas, and Las Cruces, New Mexico. This city has the second-highest volume of PWID in Mexico, with an estimated 10,000 of them (Censida, 2010), among whom HIV prevalence is estimated at 7.7% (Bautista et al., 2012).
A better understating of factors affecting drug users’ decisions about the transition to injection use and the context in which such transitions take place can inform policies on effective preventive strategies, enhancing harm reduction programs targeting non-injecting drug users before their transition into injecting as a critical component in HIV and HCV epidemic control efforts (Vlahov, Fuller, Ompad, Galea, & Des Jarlais, 2004; Werb et al., 2018).
This paper sought to compare the characteristics of transition to injection of PWID from Hermosillo and Ciudad Juárez. Specifically, this study aims to 1. determine which substances were most frequently involved in PWID initiation to injection comparing by city, and 2. to identify factors associated with faster rates of transition from first illicit drug use to the first injection among a sample of PWID.
Method
Study design and subjects
Data collection is part of a cross-sectional survey supported by the Global Fund to Fight AIDS, Tuberculosis, and Malaria (Round 9) to evaluate HIV risk among PWID in Mexico’s Northern region. A total of 841 participants were surveyed in Ciudad Juárez (n = 445) and Hermosillo (n = 396) during 2012 in places that PWID attended (hotspots), following a time-location sampling methodology.
Procedure
This sampling method involved a previous process of mapping the sites and enumerating the population in each of them to select the meeting points with larger attendance of PWID (Bautista et al., 2012). The list of the identified hotspots constituted the sampling frame. The field team visited each spot, and PWID attendees were counted. Spots were classified into small ones (with an attendance of fewer than 100 people) and large ones (with an attendance of more than 100 people), and a sample size proportional to each type of spot was assigned. The selection of small sites was made through systematic sampling, and all large sites were included. We selected potential participants randomly within each hotspot and then screened them to verify if they met the eligibility criteria (Bautista et al., 2012).
Trained interviewers with experience working with PWID collected the surveys in Spanish. The questionnaire includes sociodemographics, sexual and drug use risk behaviors, drug use and treatment history, and exposure to health facilities. On average, completing the survey took 20 minutes.
Measurements
Interviewers queried participants about their lifetime use and onset age of the following substances: inhalants, marihuana, cocaine, heroin, methamphetamines, psychedelics, barbiturics, opioids, and other prescribed medicines.
We determined the chronological year of onset and the first injection for each substance using age and date of birth. The chronological years were compared to the year of the first injection to determine which events preceded injection initiation. Cases with missing information about the entire calendar of drug use were dropped from the analysis (n = 1 from Hermosillo and n = 2 from Ciudad Juárez). The final sample obtained were 838 PWID (395 from Hermosillo and 443 from Ciudad Juárez).
The questionnaire also asked for some characteristics of first drug injection, such as the injected substance, type of assistance received, location, and if he/she was with other persons at the event. Each characteristic was included as a dummy variable in an adjusted Cox model.
Statistical analyses
We employed a Chi-Square test for categorical data and a T-test for continuous variables to compare sociodemographic, behavioral, and context-related characteristics of the sampled individuals by city.
We reconstructed drug use events for each subject from initiation age (minimum ten years) up to current use. The resulting person-year database had many lines per subject, with outcome coded 0/1, being 1 the age of first use of each substance.
First, we described the type of drug used at onset and first injection and some characteristics of the context in which the first drug injection took place, comparing by city. Second, using life tables, we analyzed the timing at first drug use and first injection. We also calculated years (duration-time) between first drug use and first injection by city.
Life tables allow us to calculate survival and probability to live the events at different ages. The benefit of a life table approach is that it does not assume a function; instead, it estimates the shape of the schedule of completing the interval. The survival function assigns each point in time a value that is the proportion of respondents in the cohort who have not experienced the event of interest, i.e., the non-use of each substance. One minus the value of the survival function is the lifetime prevalence of use at that time point. The hazard function estimates the rate of occurrence of the event within a period among those estimated not to have undertaken the event during the interval, i.e., the incidence of drug use during the period (Pressat, 2000). The unit of analysis is the age of the individuals measured in years since their birth until the age at onset of illegal drug use and first injection. Since these data were obtained in a cross-sectional survey and the eligibility criterion was having injected drugs, all the intervals are closed (that is, ranges terminated by age at onset drug use and first injection).
The sample of this study are people who inject drugs, which could provide younger timing at first injection and onset of drug use. To minimize the bias from this source, we run the survival analysis with a subsample of participants aged 25 or more (n = 679), aiming to give all individuals the same exposure time to have the event.
We established eight years old as the minimum age for the onset of illegal drug use because only four participants affirmed living the beginning of illicit drug use before this age. Likewise, we set 30 years old as the maximum age for use initiation since only six participants declared having lived the event after this age. We determined ten years as the minimum age for first drug injection (only two participants stated living the event at age nine) and 45 years old as the maximum age for this event since only four participants stated have living the event after this age. Even though some research has shown that some people initiate drug use later in life (Arreola et al., 2014), the ethnographic approach in the field (Ospina-Escobar, 2018) indicates that this is not the case of the specific sampled population.
Finally, we adjust a Cox regression model to analyze the factors associated with the transition rate from first illicit drug use to first injection. Demographic variables included age, city of residence (Ciudad Juárez vs. Hermosillo), education (secondary and above vs. less), age at first drug use, receiving assistance at first injection, and type of drug used at the onset.
Our central hypothesis states that the type of substance used at the onset of drug use is associated with the age at first drug injection. Specifically, we wanted to compare the calendar of first injection among people who initiated their drug use trajectories with substances that cannot be used by injecting versus those who began their trajectories with substances that can be injected. To make this comparison, we created a dummy variable for the type of drug use at onset, using the Pan American Health Organization classification of substances (PAHO, 2008) CODAR vs. No-CODAR, which denotes those substances that increase the risk of HIV, such as cocaine, heroin, and methamphetamine versus those that are not related with injecting practices, such as marihuana, inhalants, barbirturics, and psychedelics.
We ordered the ages at first use of each substance and identified the first substance with which the drug use trajectory began. This ordering of the events that make up the substance use trajectory from the first substance used to the last reported at the survey (Ospina-Escobar, 2016b). When the substances were grouped into the CODAR vs. Non-CODAR categories, the one that took place at the youngest age was selected for the starting substance.
The proportional hazards assumption was evaluated for the demographic variables by examining the Kaplan-Meier log-log survival curves for non-parallelism (Cleves, Gutiérrez, Gould, & Marchenko, 2010). None of the independent variables violated the assumption.
Etical considerations
All participants signed an informed consent form. Study participants were at least 18 years old, reported having injected drugs at least once during the last three months, and reported being permanent residents of the selected cities. The Institutional Review Board of the Mexico National Institute of Public Health (Instituto Nacional de Salud Pública, INSP) approved the study (CI:1011, No.1159; Bautista et al., 2012).
Results
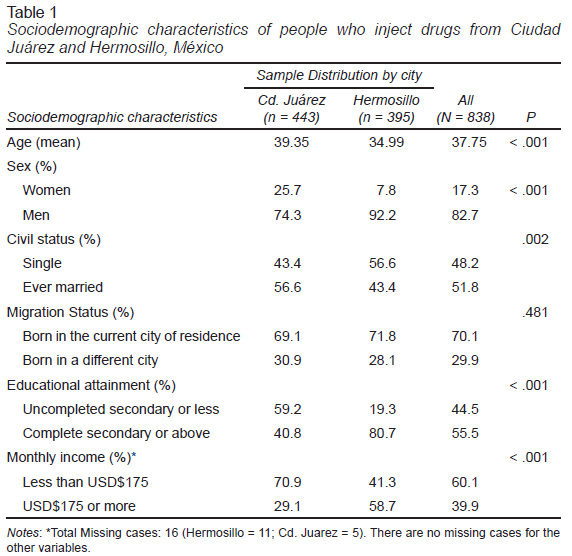
This analysis held a total of 838 participants. Table 1 presents descriptive data. 82.7% (n = 693) were men and 17.3% were women (n = 145). 52.9% (n = 443) of the participants lived in Ciudad Juárez and 47.33% (n = 395) in Hermosillo. The median age of participants was 37.75 (standard deviation [SD] 8.84). Participants from Hermosillo reported higher education and higher monthly income than those from Ciudad Juárez.
3.1 Trajectories of illegal drug use
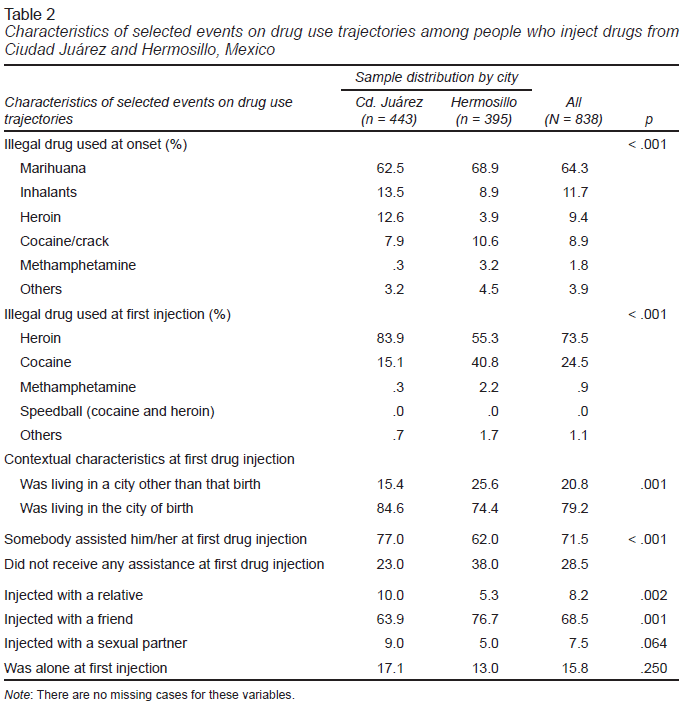
The median age for the onset of illicit drug use was 15.48 years (SD = 5.73), with significant differences between cities (p = .005). Those from Hermosillo reported an earlier onset (14.71 years; SD = 3.60) than those from Ciudad Juárez (15.94 years; SD = 6.63). Table 2 shows that marihuana was the primary illegal drug used at the onset in both cities, but the proportion was marginally higher among participants from Hermosillo (68.86% vs. 61.48%; p < .001). Interestingly, almost 13% of respondents from Ciudad Juárez reported having initiated their drug used trajectories with heroin, while the proportion was nearly 4% among Hermosillo respondents (p < .001). By contrast, 10.52% of the participants from Hermosillo used cocaine or crack at the onset of drug use, while the proportion for those from Ciudad Juárez was 7.91% (p < .001). Around 19% of the participants initiated their drug use trajectories with cocaine, methamphetamine, or heroin, without statistically significant differences by city.
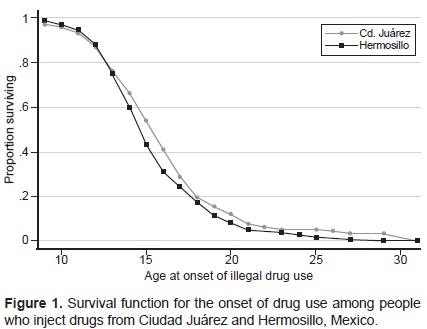
Figure 1 displays the survival function for the onset of drug use (proportions of the remaining never-users in each year of life) run only with those aged 25 or more (n = 679). Among this subsample, the rate of onset for any illicit drug use begins to climb at around age ten and reaches a peak of .50 at age 14, with the sharpest drop-off at ages 13-17. Comparing by cities, Hermosillo shows a higher residual rate of initiation at ages 12-14 and later, at ages 20-29, while participants from Ciudad Juárez show a higher residual rate of initiation at ages 16-18 (p = .04).
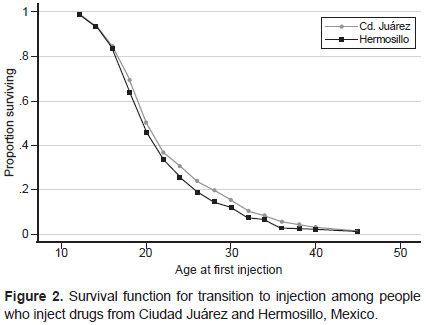
Transition to injecting
The median age at first illegal-drug injection was 21.30 (SD = 7.22), approaching significant differences between cities (p = .072). Participants from Hermosillo reported an age of transition to drug injecting one year earlier than that reported by participants from Ciudad Juárez (20.74 [SD = 6.92] vs. 21.62 [SD = 7.38]). Figure 2 displays the survival function of the remaining never-injecting who begin injecting in each year of life. The transition rate to injection reaches a peak of .50 at age 19; at age 30, 75% of respondents have lived the event with the sharpest drop-off at ages 19-22.
Regarding the characteristics of the first injection, Table 2 shows that the primary drug used at this event was heroin. Nevertheless, the proportions were significantly lower in Hermosillo (40.79%) than in Ciudad Juárez (83.93%) (p < .001). By contrast, cocaine was more prevalent in Hermosillo as the first illegal drug injected than in Ciudad Juárez (40.79% vs. 15.05%, respectively, p = .000). No participants reported heroin combined with cocaine at the onset of injecting, but 17.5% of respondents from Hermosillo and 28.1% from Ciudad Juárez declared using this combination regularly during the year prior to the survey. Remarkably, a higher proportion of participants from Hermosillo reported being migrants at first injection (25.6% vs. 15.4%, respectively; p = .001).
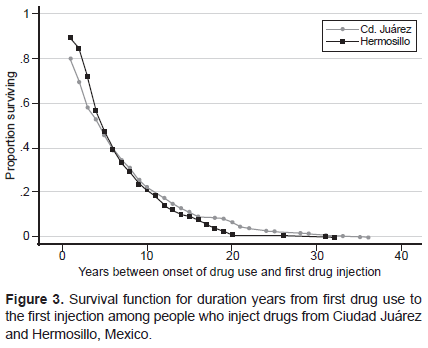
The median duration in years between the onset of drug use and transition to the first injection was 4.8 years (SD = 5.6), with no significant differences between cities (p = .51). Figure 3 displays the survival function of transition to injecting, not in calendar years, but years between the onset of drug use and first drug injection. Notably, 16.5% of the sample reported the same age at the onset of drug use and first injection, and in 7.0% of the cases, the onset of drug use was drug injection.
The transition rate to injection reaches a peak of .50 at four years since the onset of drug use. At year nine of onset of drug use, 75% of respondents had transitioned to injecting. The analysis of the transitions studied here indicates that, although the ages of onset of drug use were different between Ciudad Juárez and Hermosillo, transition to injected drug use occurred similarly over calendar-time in both cities.
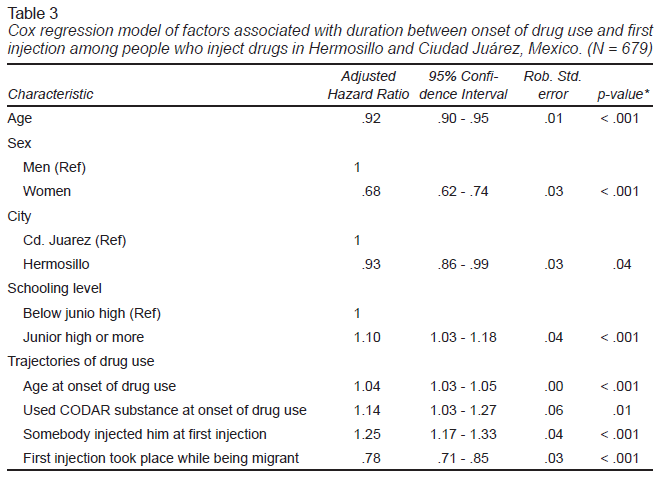
The Cox regression model (Table 3) shows that, when controlling for sociodemographics, the factors that increase the hazard of transitioning to injection from first illicit drug use are age at onset of drug use (adjusted hazard rate [AHR] = 1.04, 95% CI [1.03, 1.05], p < .01) having used a CODAR substance at the onset of drug use (AHR = 1.14, 95% CI [1.03, 1.27], p = .01) and having received assistance at first injection (AHR = 1.25, 95% CI [1.17, 1.33], p < .01).
Importantly, during the time from onset of drug use, the hazard of transition to injection for an individual who initiated his/her drug use trajectory with cocaine, heroin, or methamphetamine was 1.14 times the hazard for a person who had commenced with non-CODAR substances, adjusting for age, city of residence, and education.
Living in Hermosillo compared to living in Ciudad Juárez (AHR = .93, 95% CI [.86, .99], p = .04), being a woman (AHR = .68, 95% CI [.62, .74], p < .01) and being a migrant at the time of the first injection (AHR = .78, 95% CI [.71, .85], p = .03), were characteristics negatively associated with the hazard of transition to injection.
Discussion and conclusion
This is the first study comparing data about the onset of drug use and transitioning to injecting among PWID in a Mexican city other than Tijuana. The analysis showed substantial differences between Hermosillo and Ciudad Juárez in the type of substance used at the onset of drug use and the transition to injection. While in Ciudad Juárez, heroin was the third substance used at the onset of drug use, in Hermosillo, only almost 4% of participants reported having initiated their drug use trajectories with heroin, but cocaine was the second most prevalent substance used at this event. In the same way, although heroin was the most used substance at first injection in both cities, almost 41% of participants from Hermosillo reported cocaine as the first drug injected, but it was only mentioned by 15% of participants from Ciudad Juárez.
Despite the plausibility that drug market changes influence injecting initiation experiences, few studies have examined this topic (Horyniak et al., 2015). Our findings regarding the differences in the type of substance used at the onset of drug use and the transition to injection between Ciudad Juárez and Hermosillo could be attributed to the alien presence of criminal organizations in both cities and how they control the local drug markets.
Ciudad Juárez has a long history of drug smuggling, and its prevalence of injecting drug use and heroin use is higher than the national level since the first epidemiological data were collected back in the 1990s. Therefore, heroin has been more historically available than in Hermosillo, and that people who use drugs in Ciudad Juárez are more familiar with heroin users than users from Hermosillo. In addition, ethnographic work conducted in Ciudad Juárez showed that until 2015 methamphetamines were not available (Secretaría de Salud, 2020; Villatoro-Velázquez et al., 2012; Villatoro-Velázquez et al., 2017), and people who tried to buy or sell them were killed by local gangs that controlled the drug market (Ospina-Escobar et al., 2018).
On the other hand, Hermosillo has been controlled since the early 1990s by the Sinaloa Cartel, the leading criminal organization that traffics cocaine to the United States (Astorga, 2016). Hermosillo is also an obligatory path-point between the Pacific Ocean - from where substantial amounts of cocaine are introduced to Mexico from Colombia - and Arizona (Astorga, 2016). This geographic position could explain the greater availability of cocaine in Hermosillo’s local drug market.
Data also confirm the high availability of cocaine in Ciudad Juárez and Hermosillo in 2012, as most participants reported using it regularly alone (23.8% in Ciudad Juárez and 26.6% en Hermosillo or combined with heroin (28.1% and 17.5%, respectively).
In line with the studies that show an increasing prevalence of methamphetamine use in Sonora since 2000 (Centros de Integración Juvenil [CIJ], Sistema de Información Epidemiológica del Consumo de Drogas [SIECD], 2021; Secretaría de Salud, 2020), Most participants from Hermosillo reported having used crystal-meth at least once during the year before the survey (53.3%), and almost one third injected this substance combined with heroin (28.5%). Nevertheless, our findings suggest that methamphetamine was not widely spread as an initiation substance before 2012 (Ospina-Escobar, 2016b). More research is needed to better understand the trends of methamphetamine use in Hermosillo at the once of drug use and at the transition to injecting.
In this analysis, we reconstruct the trajectories of drug use using the events that took place before 2012, which could explain the low percentage of users who declared methamphetamine as the substance used at first injection in Hermosillo.
The difficulty of getting heroin in local drug markets in Hermosillo (Ospina-Escobar, 2019) could be explained by its geographic allocation far away from the zones of poppy crops and not in the routes for heroin smuggling (Medel, Lu, & Chow, 2015). Nevertheless, we could not demonstrate significant differences by cities in the duration time between first drug use and first injection.
The Cox regression model showed that prime factors associated with a shorter duration between onset of drug use and transition to injection are the type of substance used at onset and having received any assistance at first injection. The hazard of transition to injection for an individual who initiated his drug use trajectory with CODAR substances (cocaine, heroin, or methamphetamine) was 1.14 times the hazard for a person who had initiated with other substances for each year from the onset of drug use, adjusting for age, sex, city of residence, and education. As methamphetamine has become a significant substance used throughout Mexico (Secretaría de Salud, 2020), further explorations are required to analyze possible differences in the calendar of transition to injecting among people who use mainly heroin and those who use mainly methamphetamine, as other studies have shown (Koozegar et al., 2018).
The survival function analysis showed that among our sample, the rate of onset for any illicit drug use begins to climb at around age ten and reaches a peak of .50 at age 14. Among the general Mexican population, 15 years old is the peak age for the onset of drug use (Ospina-Escobar, 2016a). Although drug use is a practice reported only by 10% of the Mexican population, these findings reinforce the need for drug prevention and harm reduction programs targeting youth.
Our analysis showed that around 19% of participants initiated their drug use trajectories with cocaine, methamphetamine, or heroin, without statistically significant differences by city. Remarkably, 16.5% of the sample reported the same age for the onset of drug use and first injection, and in 7.0% of the cases, drug use is drug use. This finding confronts the conception of trajectories of substance use as a progressive and hierarchical sequence of involvement, posited by the gateway hypothesis (Valenzuela & Fernández, 2011). According to our findings, PWID develop other trajectories that do not match the gateway hypothesis and require a more sophisticated understanding.
Nevertheless, there seems to be a gap between 1-9 years between the onset of drug use and the transition to injection in most cases. For the 50% of the sample, the transition to injecting was within five years from the first drug use, which is consistent with other studies worldwide (Abelson et al., 2006; Ambekar et al., 2019; Bluthenthal et al., 2017; Brecht et al., 2008; Crofts et al., 1996; Doherty et al., 2000; Oliveira et al., 2006). This time lag is critical to mobilize appropriate prevention efforts and harm reduction intervention to avoid the transition to injecting, considering the specific dynamics of drug use within each city.
Our analysis indicates that although the ages of onset of drug use are different between Ciudad Juárez and Hermosillo, transitions to injected drug use occur similarly over time in both cities regardless of the diverse control exerted by criminal organizations on local drug markets. This finding could mean that motivations to injecting could be associated with the political economy of drug use (Bourgois, 2003; Ben Hamida et al., 2018; Mittal et al., 2019) which involves the sharing of knowledge and the provision of assistance among younger and older drug users with different trajectories of drug use.
This study has some limitations. First, as we collected data where PWID gather, the samples may have higher homogeneity levels among participants than the overall PWID populations in each city. As such, findings cannot be generalized to the broader population of PWID in Mexico. There is no comparative group of people who used drugs but did not transited to injecting, so we do not have a complete picture of drug use trajectories among a more diverse universe of drug users. Time to injection is only measured in years, precluding a more detailed analysis of the events analyzed.
The cross-sectional nature of the survey data also limits our capacity to detect causal associations. Other sources of bias of the data are recall bias, self-reported data, and socially desirable responses.
Even though data were collected in 2012, this is the latest available information about PWID in Hermosillo and Ciudad Juárez, suggesting the findings are still relevant for the cities and populations under study. In Ciudad Juárez, the National Institute of Psychiatry conducted a study among PWID between 2017 and 2018 and reported similar sociodemographic characteristics, ages of onset of drug use, and at first injection, along with identical drug use dynamics (Fleiz-Bautista et al., 2019).
Our data show a notable prevalence of cocaine use in Hermosillo. Nevertheless, official data about drug use trends report the decreasing of cocaine and the climb of methamphetamine use since 2006 (CIJ & SIECD, 2021; Villatoro-Velázquez et al., 2012). The high prevalence of cocaine use in Hermosillo could be related to the better socioeconomic status reported by participants from this city than participants from Ciudad Juárez, which is indicated by their monthly incomes and education attainment (Table 1). Participants from Hermosillo also reported lower access to treatment for drug abuse and more affluent contacts with social networks that facilitated access to a more diverse universe of substances including cocaine (Ospina-Escobar, 2016b).
Given the scarcity of data available, there is an urgent need to better understand the trajectories of drug use among PWID and translate this understanding into the design of programs, strategies, and public policy to treat problematic drug use and consolidate the offer of harm reduction services in Mexico.
Shortly, we can conclude that the early onset of drug use, along with the association found between methamphetamine as a starter substance at the onset of drug use and the faster transition to injection, lead us to conclude that increased use of crystal-meth in Mexico is highly likely to lead to an increase in the volume of PWID in the mid-term. Increasing drug injection presents significant public health challenges, including the spread of HIV and HVC. It is urgent to boost the offer of public health facilities for problematic drug use. It also should be a priority to include long-standing harm reduction programs funded by local and federal governments to address other health risks associated with injecting drugs.