INTRODUCTION
At the end of 2019, Wuhan Municipal Health Commission (China) reported several pneumonia cases in the city, which were later attributed to a new coronavirus, SARS-CoV-2, which causes COVID-19 disease. On January 13, 2020, the first case outside China was confirmed (World Health Organization [WHO], 2019). By the end of September 2020, the pandemic had already surpassed the one million death mark and more than 16 million confirmed cases in the Americas (WHO, 2020). Despite the short time since the beginning of the pandemic, there is already evidence not only of the impact of the virus on physical health (Harapan et al., 2020; Chams et al., 2020), but also on mental health. Although evidence of psychiatric and neurological sequelae, such as intracranial hemorrhage, ischemic stroke, and dementia, has already begun to be found (Taquet, Geddes, Husain, Luciano, & Harrison, 2021), the main effects on mental health have been due to indirect effects of the pandemic, such as social isolation, anxiety and uncertainty about the risk of infection (Pera, 2020; Stamu-O’Brien, Carniciu, Halvorsen, & Jafferany, 2020; Urzúa, Vera-Villarroel, Caqueo-Urízar, & Polanco-Carrasco, 2020). In general population, several reviews show evidence of the negative impact of the pandemic on mental health: higher degrees of psychological distress and anxiety, presence of depressive symptoms, sleep disorders, post-traumatic stress, lower psychological well-being, mood changes, and low self-esteem, among others (Gawai et al., 2020; Pera, 2020; Salari et al., 2020; Xiong et al., 2020; Vindegaard & Benros, 2020). These mental health problems seem to be increasing in specific populations with different types of vulnerability and risk, such as people with pre-existing mental disorders (Pera, 2020; Vindegaard & Benros, 2020), health workers (Braquehais et al., 2020; Luo, Guo, Yu, Jiang, & Wang, 2020; Pappa et al., 2020; Salazar de Pablo et al., 2020; Samaniego, Urzúa, Buenahora, & Vera-Villarroel, 2020; Shaukat, Ali, & Razzak, 2020; Urzúa, Samaniego, Caqueo-Urízar, Zapata Pizarro, & Irarrázaval Domínguez, 2020), COVID-19 patients (Pera, 2020; Vindegaard & Benros, 2020), women, unemployed individuals, and students (Xiong et al., 2020), among others.
One of the groups at the greatest risk of mental health problems and lowest rates of well-being is the gay, bisexual, and transgender (LGBT) population, a group for which a higher prevalence of mental health problems has been reported, as compared with the general population (Meyer, 2003; King et al., 2008; Stinchcombe, Wilson, Kortes-Miller, Chambers, & Weaver, 2018) since they have historically been subjected to prejudice and discrimination. According to Meyer's theory of minority stress, exposure to a hostile and discriminatory social environment may result in a greater vulnerability of certain groups highly stigmatized because of their sexual orientation or gender identity (Mongelli et al., 2019; Meyer, 2003). In the case of the Chilean population, previous studies (Barrientos, Gómez, Cárdenas, Guzmán, & Bahamondes, 2017) report that 9% of gay men and 12% of lesbian women score above the cut-off point in anxiety-depression, without finding significant differences between gays and lesbians in this dimension. Likewise, a study on Chilean transgender population showed that 40% of the participants had been diagnosed with depression and the averages of symptoms of depression, anxiety, and stress were higher than the cut-off values established for young Chilean population (Guzmán-González et al., 2020).
Currently, there are still few specific reports on this population in the context of COVID-19. A study by Suen, Chang, and Wong (2020), conducted in Hong Kong, reported that 31.5% of the participants met the criteria of a probable clinical depression and 27.9% of generalized anxiety disorder, concluding that stress factors specific to sexual minorities in the context of COVID-19 contributed significantly to explain the symptomatology variance, beyond the contribution of the stressors associated with COVID-19. A second study, conducted through the Hornet social network on more than 2,000 participants from various countries, found that 35% of them presented symptoms for depression and 34% for anxiety, with job loss being one of the main factors associated with both disorders (Santos et al., 2021). A third study, conducted on 1,051 men who have sex with men living in the United States, reported that 71% of the participants had increased their anxiety symptoms during this period (Sanchez, Zlotorzynska, Rai, & Baral, 2020). Further evidence was provided by a recent OutRight Action International (2020) carried out by several countries during the COVID-19 pandemic through literature review and interviews. This report shows a high risk of domestic violence, social isolation, and increased anxiety, among others, during this pandemic in the LGBT population. For example, many LGBT young adults have not disclosed their sexual and gender identities to their families or lack support and acceptance from their primary socialization group (Ryan, Russell, Huebner, Diaz, & Sánchez, 2010). This is because families of origin often reflect the existing wider societal stigma and become a source of discrimination for LGBT individuals, increasing mental distress not only during adolescence but also into young adulthood (Ryan et al., 2010).
In this context, this work aims to describe the prevalence of symptoms associated with mental health disorders, as well as to analyze the risk of their occurrence, in different groups of the Chilean LGBT population in the context of COVID-19.
Considering the results of previous studies in the LGBT population, it is expected as a hypothesis to find differences within the different groups that make up this population, where the population who reported themselves as bisexual would have worse mental health than those who define themselves as homosexuals (gays and lesbians; Chan, Operario, & Mak, 2020; College, Hickson, Reid, & Weatherburn, 2015; Ross et al., 2018).
METHOD
The study was carried out under an observational design of a cross-sectional analytical type.
Participants
A total of 1,189 people completed surveys through an intentional online sampling. All of them were over 18 years old and self-identified as belonging to the LGBT population. For the analysis purpose, from the total number of questionnaires received, seven were eliminated because the individuals self-identified as heterosexual.
Instruments
Sociodemographic measures
The first part of the questionnaire collected information such as socio-demographic data, age, sex assigned at birth, gender identity, sexual orientation, educational level, and occupational status.
Mental health measures
The depression Anxiety Stress Scales (DASS-21) were used to evaluate anxiety, depression, and stress (Henry & Crawford, 2005; Lovibond & Lovibond, 1995a; 1995b) in its Spanish versions (Daza, Novy, Stanley, & Averill, 2002). To establish the cut-off points, the recommendations of the study conducted on Chilean population were followed (Román, Santibañez, & Vinet, 2016). For the Depression Scale, a cut-off point of 6 (> 5) was used; for the Anxiety Scale, the cut-off point corresponded to 5 (> 4), and for the Stress Scale, a cut-off point of 6 (> 5) was used. The reliability of the total scale in this study, evaluated with Cronbach's alpha statistics, was .95, while for the subscales it was .91 for depression, .86 for anxiety, and .88 for stress.
Procedure
Considering that this is a population of which the universe is unknown, a combination of the respondent driven sampling method (Cárdenas & Yañez, 2012) with an intentional sampling was used to gather information, linked to the LGBT population. The link of the questionnaires was sent to various seed persons and institutional networks from different universities and the sexual diversity movement, who distributed them among their networks. At the same time, the link was disseminated by various social networks such as (Instagram & Facebook). Since it was a convenience sample, carried out through an online sampling, nobody was excluded from participating. The questionnaires were administered online between mid-June and mid-July 2020. Data was collected through the Google Forms platform, which exported data to an Excel spreadsheet. Data were then changed into an SPSS.25 database for analysis.
Statistical analysis
First, the central tendency measures of the studied variables were analyzed, and then the cut-off points suggested by Román et al. (2016) were used to establish prevalences according to sex and sexual orientation. Differences in means between the groups (based on sexual orientation) in each of the symptoms were subsequently analyzed using ANOVA, with post-hoc contrasts with the Scheffé method, controlling the analyzes by age and income as covariates. Finally, the probability of symptoms was analyzed using odds ratio.
Ethical considerations
Before starting data collection, the project was reviewed and approved by the institutional committee of scientific ethics of the Alberto Hurtado University (Resolution without number 2019). All participants had to sign an informed consent online, where the voluntary nature of participation was raised, prior to completing the questionnaires. The instruments were filled out anonymously.
RESULTS
Participants
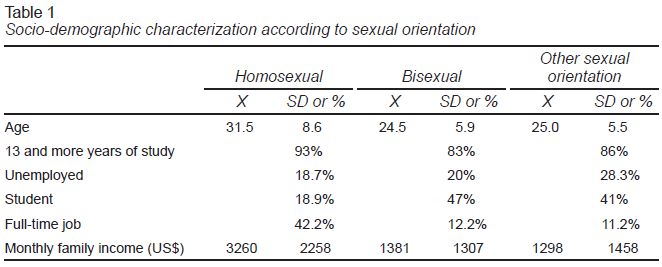
From the 1,181 participants, 58% identified themselves as male, 40% as female, and 2% as non-binary. In terms of sexual orientation, 64% defined themselves as homosexual (HS; n = 758), 23% as bisexual (BS; n = 271), and 13% as other sexual orientations (OSO; pansexual, demisexual, asexual, other; n = 152). Participants’ age ranged from 18 to 64 years, with a mean of 29 years (SD = 8.4), a median of 28 and a mode of 23 years. The questionnaire was completed by people from all the administrative regions of the country. Table 1 shows the sociodemographic characterization of the participants.
Mental health symptomatology
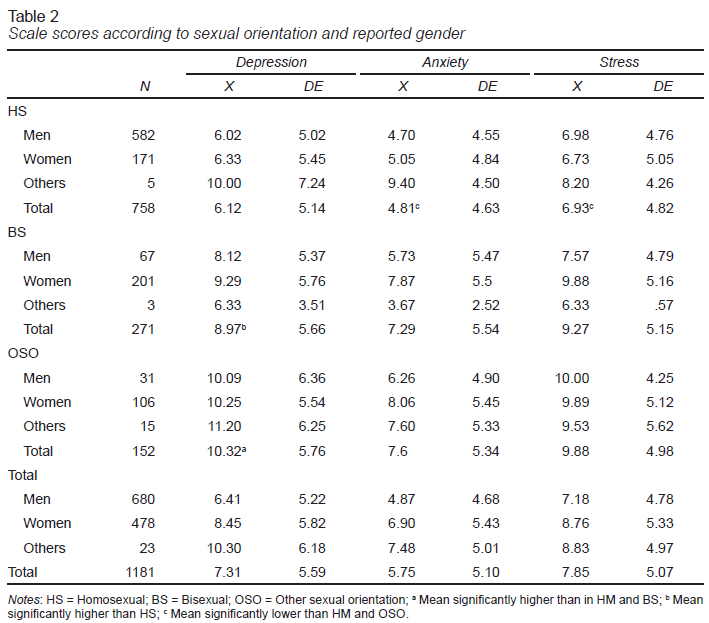
Table 2 shows the scores obtained in the different groups for each of the symptoms evaluated.
There are significant differences in the scores of depressive symptoms in the means of the three groups (F [2,1178] = 55,958; p = .000; η2= .087), a difference that is still significant controlling by age (F [1] = 47,868; p = .000), income (F [1] = 10.641; p = .001), and educational level (F [1] = 4,505; p = .034). When analyzing these differences, the mean for the group that reports itself as OSO is significantly higher than those who report themselves as bisexual (p = .039) and homosexual (p = .000), the latter being significantly lower than that of bisexuals (p = .000).
In the case of anxiety, there are also differences between sexual orientations (F [2,1178] = 37,903; p = .000; η2 = .060), which are controlled by age (F [1] = 39,014; p = .000) and income (F [1] = 356,267; p = .000). Here, the average of the group that reports itself as homosexual is significantly lower than that of the group of bisexuals and OSO (all differences with a p = .000), but only in those who have 13 or more years of study.
In the symptomatology associated with stress, there are also significant differences between the groups (F [2,1178] = 37,460; p = .000; η2 = .060), which are also controlled by age (F [1] = 51,160; p = .000) and income (F [1] = 187,032; p = .004). Also, the mean of the group reporting itself as homosexual is significantly lower than that of the bisexual and OSO groups (all differences with a p < .001), but also only in those who have 13 or more years of schooling.
Symptomatology prevalence
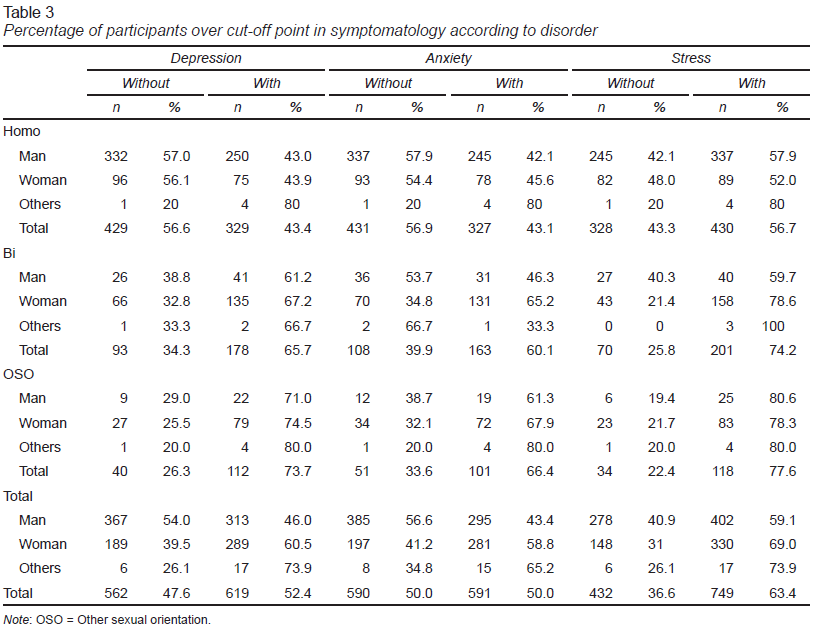
When using the cut-off points considered for the possible presence of a disorder (Table 3), results show that, in general, these are high, even reaching percentages above 70% in the case of the OSO population, for participants with values above the cut-off point in depression and stress. OSO show a ratio of people above the cut-off point higher than those reporting themselves as bisexual and homosexual. Similarly, bisexuals show a greater ratio of people over the cut-off point than gays and lesbians.
Risk of occurrence by group
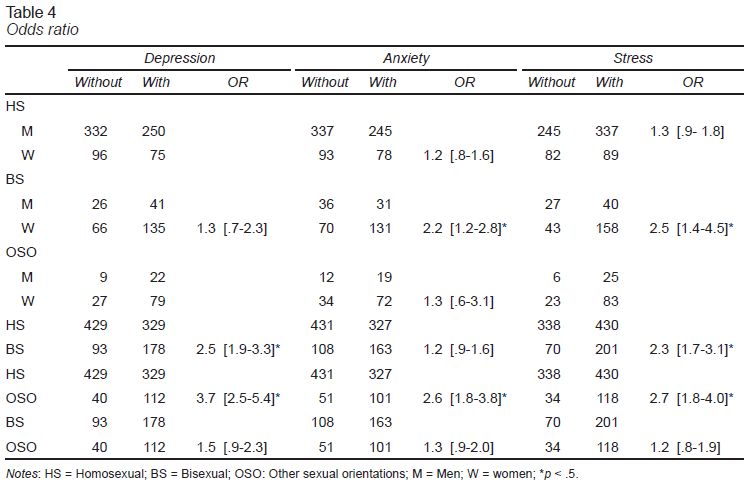
The odds ratio analysis (Table 4) shows that the risk of presenting depressive symptoms in the bisexual population is 2.5 times higher than that of homosexuals, rising to 3.7 in the case of OSO compared to the homosexual population.
In the case of anxiety, bisexual women have a significantly higher risk than men with a similar orientation. Similarly, the OSO population has a significantly higher risk than the homosexual population of presenting depressive symptoms. In the case of stress, women have a significantly higher risk than men of presenting symptoms, as do bisexuals and OSO population compared to homosexuals.
DISCUSSION AND CONCLUSION
This study evaluated the mental health status of a sample of Chilean LGBT adult population during the COVID-19 pandemic. The results show an increased risk during the COVID pandemic, considering the current vulnerability of this population due to their sexual orientation or gender identity.
In general terms, and even though we cannot establish causality, we have found that the prevalence of symptomatology in the evaluated population is notably higher than that reported in similar population in previous studies (Barrientos et al., 2017), a rise that, given the research evidence in diverse populations, could have its cause in the pandemic.
We have likewise found differences by sexual orientation. Participants who self-identified as homosexual (both men and women) present fewer depressive symptoms than those who self-identify as bisexual and the OSO population, the latter more than bisexuals. A similar situation is found in anxiety and stress, where the mean of the group that self-defined as homosexual was significantly lower than that of the other groups, but only in those who reported 13 or more years of schooling. Likewise, when comparing the risk of presenting symptomatology by sexual orientation, the results show that bisexuals are more likely to have depressive symptoms and stress than those who declare themselves homosexual. Similarly, bisexuals show a higher proportion of people above the cut-off point than gays and lesbians. In terms of percentages, OSO show a higher proportion of people above the cut-off point than those who declare themselves bisexual and homosexual. Additionally, the OSO population presents a significantly higher risk of presenting depressive, anxious, and stress-related symptomatology than the homosexual population.
This disparity within the LGBT population is like that found in Hong Kong by Chan et al. (2020) who reported that those who described themselves as bisexual showed higher levels of depressive symptoms and anxiety than lesbians and gay men. Although some studies do not find these differences (Balsam, Beauchaine, Mickey, & Rothblum, 2005), Ross et al. (2018) conducted a systematic review and meta-analysis concluding that there is a lower prevalence of depression and anxiety in heterosexuals, while bisexuals show higher or equivalent rates compared to lesbians and gays. Explanations that could underpin these inequalities include experiences of discrimination based on sexual orientation (being discriminated against by both heterosexual and homosexual populations), bisexual invisibility, and lack of affirmative support for bisexuality (Ross et al., 2018). Chan et al. (2020) give a similar explanation, finding greater identity uncertainty, concealment of sexual orientation, and less connection to the LGBT community as possible causes. The approach of greater discrimination towards bisexuality (especially in the case of women) is discussed, as there is evidence that bisexual women might be less stigmatized because they are less visible to society and more heterosexual than lesbians (less deviation from the norm; College et al., 2015; Sarno, Newcomb, Feinstein, & Mustanski, 2020). Similar findings are reported by Dyar, Feinstein, and London (2015) who, comparing bisexual and lesbian women, found that lesbians show greater sexual identity centrality, externality, and accuracy of self-perception of their sexual identity label, whereas bisexual women report greater uncertainty about their sexual identity. The same is reported by Puckett, Surace, Levitt, and Horne (2016), who found that lesbians report greater victimization, discrimination, and expectations of discrimination than bisexual women, with the latter having higher levels of identity concealment and greater internalized heterosexism than lesbian women. Although we have not come across findings for comparison purposes in the population we have called OSO, it is possible that the higher risk of presenting greater symptomatology than the homosexual population is also given by the invisibility of these sexual practices, identity uncertainty and a lower connection with the LGBT community, as found in the bisexual population (Chan et al., 2020).
When assessing the probability of presenting symptoms above the cut-off point, bisexual women show a higher probability of presenting symptoms associated with mental health disorders than men. Similar findings are reported by College et al. (2015), who found that bisexual women report worse mental health and more psychological problems than lesbians, suggesting that bisexual women may be more likely to experience social stress due to “double discrimination,” i.e., homophobia and biphobia.
In summary, we have found that there is a high prevalence of symptomatology associated with mental health disorders (higher compared to previous studies without COVID), that the bisexual and especially OSO populations have a higher presence of symptoms than the homosexual population, and finally that in the bisexual population, women have a significantly higher risk of presenting anxious and stress symptoms than men. The results highlight the disparities within the different LGBT communities, showing the need to focus on preventive interventions and the implications of higher risk in the bisexual population and particularly in women, who are affected by various cross-discriminations.
The results of this study must be interpreted considering certain limitations. Given the cross-sectional nature of data collection, it is only possible to report but a photograph of the moment without being able to establish causalities in terms of the effect of COVID, since there is no previous history of prevalence with a similar instrument, limiting ourselves only to noting an increase. compared to previous studies. The non-probabilistic nature of the sample and a greater representation of people with high educational levels limit the generalization of the results to the LGBT population. It should also be mentioned that the information obtained through self-report measures may not necessarily coincide with the actual presence of symptoms, since there was no face-to-face clinical evaluation as a validation method, the veracity of the results based on in the psychometric properties of the instruments used. Finally, data collection was carried out online, so participation in this research was limited to the population with Internet access.