INTRODUCTION
Health professionals working in hospitals are particularly vulnerable to suffering from various psychological affectations (Duarte, Velasco, Sánchez-Sosa, & Reyes-Lagunes, 2019; Fouilloux et al., 2020; Gómez-Urquiza et al., 2017; Vidal, Chávez-Negrete, Riveros, & Sánchez-Sosa, 2019). Various complaints are associated with health system conditions (González & Pérez, 2012; Polanco et al., 2013); interpersonal dynamics at work (Brooks, Gerada, & Chalder, 2011; Aguado Martín, Bátiz Cano, & Quintana Pérez, 2013) and individual aspects (Landa-Ramírez et al., 2017; Trifunovic, Jatic, & Kulenovic, 2017). The consequences affect the quality and way of interacting with patients and other health team members, imbalance between work and personal life, and various aspects of their health (Duarte et al., 2019; Reith, 2018; Shanafelt et al., 2012).
This background has prompted the investigation of factors that can function as protectors against these consequences. Among them, resilience has gained an important role due to its apparent association with low levels of stress, anxiety, and burnout, among others (Rushton, Batcheller, Schroeder, & Donohue, 2015; Ríos-Risquez, García-Izquierdo, Sabuco-Tebar, Carrillo-Garcia, & Martinez-Roche, 2016; Deldar, Froutan, Dalvand, Gheshlagh, & Mazloum, 2018; Foster et al., 2019; Yu, Raphael, Mackay, Smith, & King, 2019).
The concept of resilience has been defined in diverse ways making it difficult to have consensual conventional concepts. This has contributed to a separation between resilience theory and practice. While there are core, widely accepted factors of resilience, such as social support (APA Help Center, 2019), others vary depending on the author and the instrument used to assess them.
Several commonalities have been found in the study of resilience (Connor & Davidson, 2003; García-Vesga & Domínguez-de la Ossa, 2013;Fernandes de Araújo & Bermúdez, 2015; Ortunio & Guevara, 2016; Stainton et al., 2019). These consistencies include perceived stress, adversity, and hostile work contexts. These contexts are not limited to extreme cases, such as losing a colleague or loved one. The context also functions as a protective factor to reduce everyday risk events, such as social, family, educational, and occupational vulnerability. When the individual successfully copes with these adversities, positive adaptation usually results.
Due to this conceptual complexity, resilience is considered a multifactorial phenomenon, where the qualities and resources of the individual contribute to the successful coping of the adverse situation (Connor & Davidson, 2003; García-Vesga & Domínguez-de la Ossa, 2013; Ortunio & Guevara, 2016). In general, resilience should be seen as a process and not only as an inherent or characteristic element of the individual (Stainton et al., 2019). Consistent with this stance, Saavedra proposed a model of resilient response from the emergent case study (Saavedra, 2003; Saavedra & Villalta, 2008, p. 32).
This approach sees resilient responses as goal-oriented actions that meet three essential conditions: a) Basic conditions, including beliefs, values, experiences, and social ties that the subject has developed throughout his or her life. b) Positive self-view, which includes positive emotions and thoughts that the person identifies in him/herself in the face of adversity, and c) Problem view, an articulated and positive perception in which the problem appears surmountable.
Several authors refer to resilience as a critical protective factor in the workplace (Jackson, Firtko, & Edenborough, 2007; Howe, Smajdor, & Stöckl, 2012; Epstein & Krasner, 2013; Brennan, 2017; Sotile, Fallon, & Simonds, 2019; McKinley et al., 2019; Yu et al., 2019). However, most studies assessing resilience use instruments with poor theoretical congruence, i.e. different elements of resilience from one instrument to another; low inter-scale consistency, and weak or absent ecological validity (measurement under specific conditions present during measurement).
Thus, it is essential to have a consistent resilience instrument with good psychometric characteristics for the population of hospital health professionals. Such an instrument would allow the proper evaluation of this protective factor and contribute to designing and examining the effectiveness of interventions that promote resilience. Within a broader study that evaluates risk and protection variables in health personnel, it was decided to use the Resilience Scale SV-RES. Due to its flexibility of use and validity of items, the objective of this study was to adapt and validate a scale to measure the resilient response of hospital health professionals.
METHOD
Design of the study
Development process of a measurement scale.
Participants
A total of 909 health professionals (attending staff and students) from the various services and shifts of the hospital participated. Participation was voluntary and strictly anonymous after signing the corresponding informed consent form. Personnel under psychiatric or psychological treatment or participating in any other study that could bias the findings were excluded from the analysis. Also excluded were those who had not responded to at least 80% of the items. The invitation to the study was open to all hospital staff and students through invitations from service chairpersons, social networks, posters, and other similar means. Seventy percent of the total staff participated, enough to be representative of said hospital. Data collection included from November 2018 to February 2019.
Measurement
The Resilience Scale SV-RES, initially developed by Saavedra and Villalta (2008) for the Chilean population, evaluates the concept of resilience-based on Edith Grotberg՚s theory of resilient verbalizations and Saavedra՚s resilient response model. It is a 60-item scale grouped into 12 factors: identity, autonomy, satisfaction, pragmatism, links, networks, models, goals, affectivity, self-efficacy, learning, and generativity. The answers require responding to a Likert-type scale, ranging from “1 = totally disagree” to “5 = totally agree”, leading to a score for each factor and a global score through the sum; a higher score greater resilience capacity.
The original Scale has internal consistency of α = .96 (Cronbach՚s alpha) and validity through Pearson՚s coefficient of r = .76, p < .05 with the CD-RISC instrument (Connor & Davidson, 2003).
Procedure
Once the original author of the scale gave the proper authorization, the scale was submitted to a trial with 24 expert health psychologists to examine comprehension (wording and structure) of the Mexican culture and to identify whether the items effectively evaluated relevant dimensions (content validity). Due to some initial inconsistencies in the results (Aiken coefficient less than .70), the next version got modified based on the most consistent suggestions stemming from the first procedure.
A second trial was carried out with 43 experts to evaluate factor assignment, adequacy to the Spanish language. Correct grammatical usage was assessed by an expert grammarian-philologist in Spanish. An interquartile deviation > 1.4 and a coefficient of variation < 30% were used as criteria for the discrimination capacity of the items, leading to a new version of 60 items.
The final version of the instrument was then administered to 909 health personnel to examine its main psychometric properties. The study is part of a larger project, the evaluation proceeded through a general battery composed of seven instruments. In order to avoid bias, the data corresponding to the resilience variable were recorded and analyzed separately. The capture and scoring of the items was carried out by means of a blind procedure and, in order to guarantee correct data capture, 30% of the captures were, again, randomly reviewed.
Statistical analysis
Sociodemographic variables were examined through measures of central tendency and dispersion.
The analysis included frequency, Kolmogorov-Smirnov Z test, asymmetry and kurtosis, to identify the directionality and distribution of the data. The discriminative power of the items was examined employing two tests: a comparison of extreme groups for the total test (first and fourth quartiles) using the Mann Whitney U test. The total correlation of the test and each item used a correlation cutoff point above .30. (Construct validity) Factor analysis used the principal axis method with oblique rotation (Fabrigar, Wegener, MacCallum, & Strahan, 1999; Ferrando & Anguiano-Carrasco, 2010; Beavers et al., 2013). To measure the relevance of the analysis, the Kaiser-Meyer-Olkin sample adequacy index (KMO = .920) and Bartlett՚s test of sphericity (X2 = 9979.492; degrees of freedom = 378; p ≤ .001) were computed. Elimination criteria included factors with two or fewer grouped items and items with factor loadings less than .40 (Morales Vallejo, 2013; Ferrando & Anguiano-Carrasco, 2010). Finally, reliability (internal consistency) was assessed through Cronbach՚s Alpha formula (Hernández, Fernández, & Baptista, 2010; Quero, 2010; Kerlinger & Lee, 2002).
Ethical considerations
This research is part of a larger one approved by the Research and Research Ethics Committee of the Hospital General Dr. Manuel Gea González, with the title of “Association of burnout with psychological and organizational variables in medical and nursing students and staff of the Hospital General Dr. Manuel Gea González”.
Registration number: 27-51-2018, August 30, 2018.
RESULTS
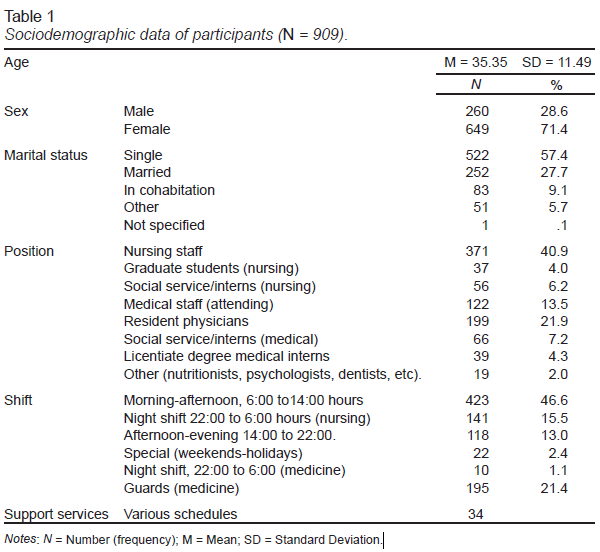
The results include data from 909 health professionals from 24 medical services and five shifts, with an average age of 35.35 years and a standard deviation of 11.49. Of the participants, 464 were students and staff from the nursing area, 426 from the medical area, and 19 from nutrition, dentistry, and psychology (Table 1).
The frequency analysis of the 60 items showed that the directionality of items 2, 3, 8, 9, 11, 14, 17, 18, 22, 23, 27, 28, 31, 35, 37, 38, 41, 42, 45, 46, 48, 52, 55, 56, and 57 was contrary to that of the rest, leading to inverting the score. In the data distribution for each item, the Kolmogorov-Smirnov Z test ranged between .178 and .370; p < .001, with negative asymmetries and leptokurtic kurtosis, indicating a skewed distribution.
Prior to the factorial analysis, item 19: “I am a person who evaluates the meaning of life in difficult moments”, was eliminated since its correlation with the total of the test was less than .30 (.249; p < .001).
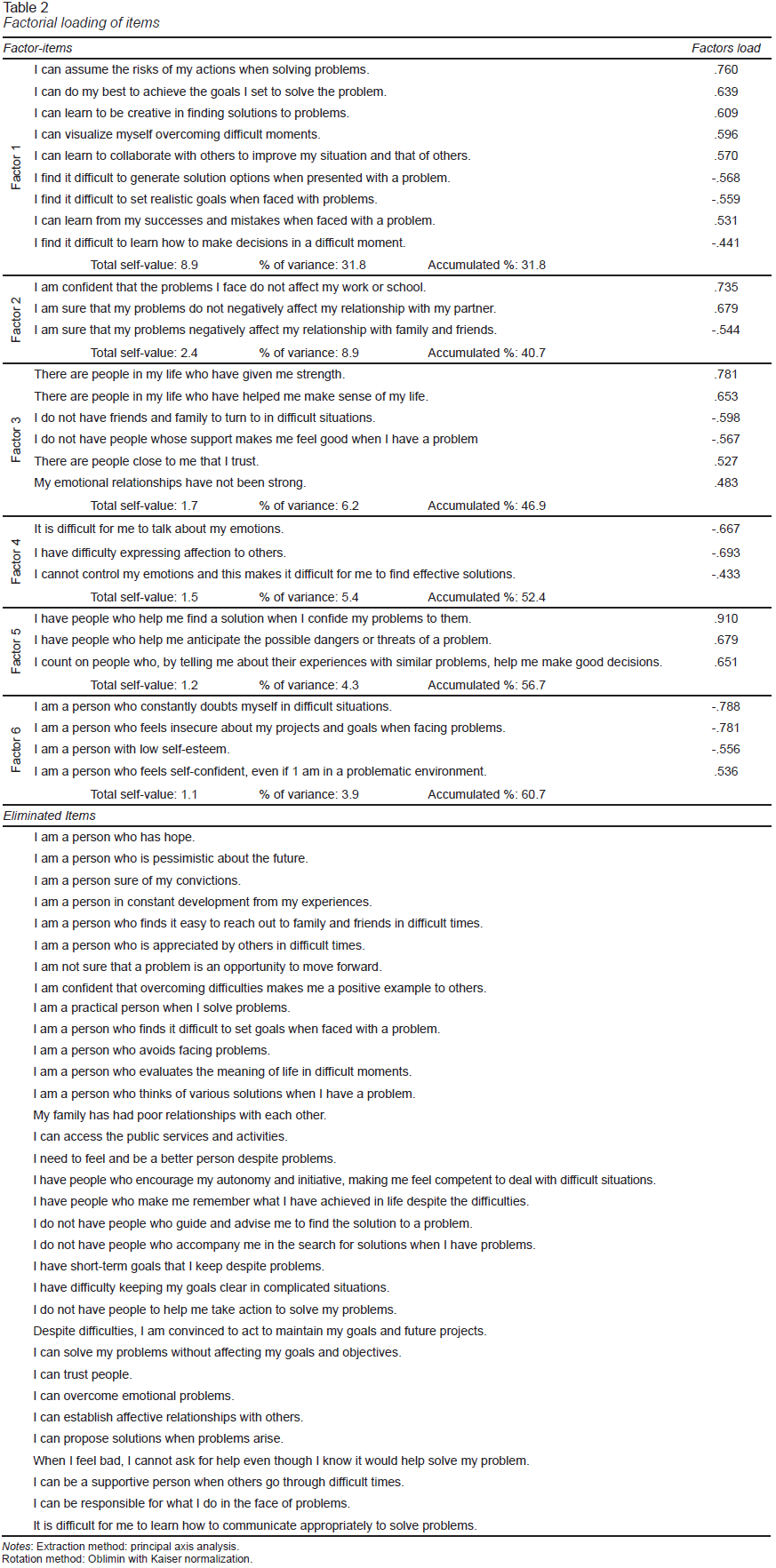
The final results of the factor analysis showed a grouping of 28 items in six factors, with loadings ranging from .433 to .910 and an explained variance of 60.7%. The first factor grouped nine items, the second, fourth and fifth with three; the third with six, and the sixth with four items. Thirty-two items were eliminated (Table 2).
Finally, the internal consistency test revealed a value of α = .908, and for each factor, the reliability index ranged from α = .708 to α = .882.
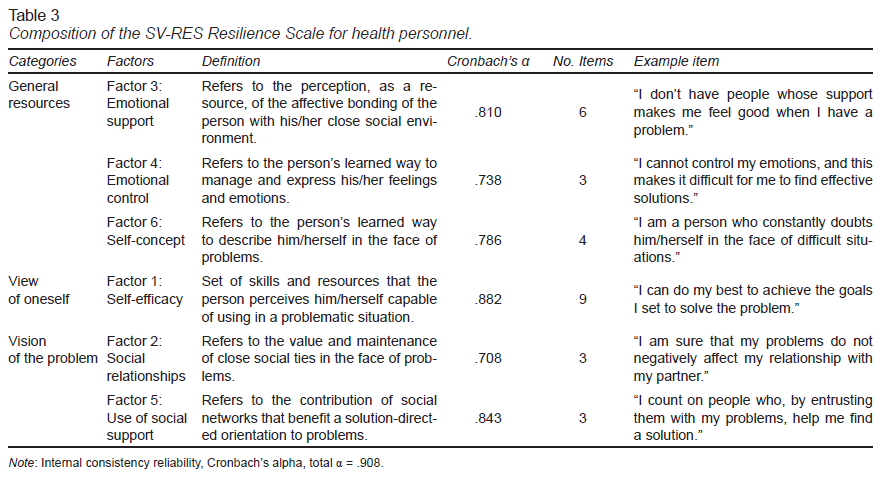
According to the characteristics of their items, the factors obtained were theoretically matched with the resilient response model which supports the original instrument, as follows; General Resources (Factor 3, 4, and 6), Vision of oneself (Factor 1) and Vision of the problem (Factor 2 and 5).
DISCUSSION AND CONCLUSION
The objective of this study was to adapt and validate the SV-RES resilience scale for Mexican hospital health professionals. The instrument has good psychometric properties; content validity, construct validity, and internal consistency.
The exploratory factor analysis led to eliminating over because their factor load did not exceed the established limit of .40 or grouped into factors with two or fewer items. This procedure left 28 items with five response options, from 1 “totally disagree” to 5 “totally agree”. The items belong to six factors, obtaining, through the sum, a total score on the resilience capacity in the face of problematic situations (resilient response) and each factor that composes it. The items whose rating is reversed are; 6,7,9,12,15,16,18,19,20,21,25, 26, and 27.
The factors were defined based on the relationship of the items and the relevant research literature (Saavedra & Villalta, 2008; Ortunio & Guevara, 2016; Stainton et al., 2019; Fernandes de Araújo & Bermúdez, 2015). The factors obtained coincide with the theoretical resilience model proposed by Saavedra, as follows: Base conditions (factors 3; Emotional support, 4; Emotional control, and 6; Self-concept), Vision of oneself (factor 1; Self-efficacy), Vision of a problem (factors 2; Social relationships and 5; Use of social support), and the score total (all factors), resilient response (Saavedra & Villalta, 2008; Saavedra, 2003; Table 3).
The identified factors describe resilience as a coping resource in widely documented situations requiring resilience as a process. They include coping, successful problem solving, and learning to resolve future conflicts (Stainton et al., 2019). This structure seeks to identify the present conditions and how they get perceived in the face of a problematic situation.
In the six factors obtained, social support, a proactive vision, self-confidence, and the management of feelings and emotions stand out (APA Help Center, 2019). Indeed, these are core dimensions to consider as pillars within the concept of resilience when seeking to homogenize the analysis of the concept in real situations and identify ways to design effective interventions. Finally, the instrument is a reliable option for assessing the resilience capacity of hospital health professionals. Also, the length of the scale will result in a shorter application time compared to its original version, which increases its viability of use in a population with work overload.
It is essential to note that this study is part of a broader one, which is why it required adaptation to the conditions set by the main project. For example, the application included a battery composed of six instruments, which extended the average answering time to 30 min, which could have influenced the participants՚ responses. This point should be relevant for future research in terms of practicality. Similarly, the present study involved an exploratory factor analysis. More exhaustive analysis (confirmatory factor analysis) would verify the factors obtained and their relationship with the three categories of Saavedra՚s resilient response model.
Finally, future research should consider the diversity of health professionals participating in these studies. The research literature generally reports high levels of resilience, but with minor differences in both students and staff (Chaukos et al., 2017; Dorote, 2018; Foster et al., 2019; McCain et al., 2017; Ríos-Risquez et al., 2016; Walpita & Arambepola, 2020; Yu et al., 2019).