INTRODUCTION
Some of the changes introduced by the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) involve the way functioning and disability are assessed. In the DSM-5, the World Health Organization Disability Assessment Schedule (WHODAS) 2.0 replaced the Global Assessment of Functioning (GAF). The DSM-5 Task Force deemed it necessary to replace GAF because of its lack of conceptual clarity and questionable psychometrics in routine practice (American Psychiatric Association, 2013).
WHODAS was created in 1988 as a self-reporting tool to record an individual’s perspective on their daily functioning. It provides a standardized score measuring difficulties in functioning in the previous thirty days, regardless of any other diagnosis (Rotter, 2018). Answering WHODAS 2.0 implies a degree of insight that could be challenging for some children. The updated version, WHODAS 2.0, is based on the International Classification of Function (ICF) conceptual framework and captures the level of functioning in six domains of life: cognition, mobility, self-care, relationships, life activities and participation. WHODAS 2.0 places health and disability on a continuum, defining disability as “a decrease in each domain of functioning” (Üstün et al., 2010). In contrast to GAF, the WHODAS 2.0 score does not explicitly consider the severity of mental illness (Gspandl et al., 2018). As WHODAS does not consider the severity of mental disorders as part of the disability/functionality dimension, it allows for the assessment of the latter when there is no correlation with symptom severity (Smith et al., 2011; Von Korff et al., 2011; Söderberg et al., 2005).
In the 3rd edition of the DSM (American Psychiatric Association, 1980), axis V was introduced as a measure of “adaptive functioning” and scored on a 7-point scale ranging from superior to grossly impaired. In the revised 3rd edition of the DSM (American Psychiatric Association, 1987), the GAF scale replaced axis V for the assessment of psychological, social, and occupational functioning. In the 4th edition of the DSM, the GAF scale was extended to a 100-point scale (Pedersen & Karterud, 2012). The GAF scale assesses patient symptoms and overall functional ability on a single hypothetical continuum of mental health-related illness (Gspandl et al., 2018). GAF can be reliable, valid, and sensitive to change over time. However, certain limitations have been widely acknowledged. GAF specifically excludes impairment in functioning due to physical or environmental limitations and scores frequently correlate more with the severity of disorders than with levels of disability (Gold, 2014).
The elimination of GAF and the incorporation of WHODAS 2.0 has posed entailed several challenges due to the differences between these instruments. While the justification for using WHODAS 2.0 to expand the evaluation of global functioning and disability (Reed, 2010) is reasonable, some questions appear unsuitable for children and adolescents (“Staying by yourself for a few days?” “Sexual activities,” “Assuming your household responsibilities” or “Getting your housework done as quickly as needed”). Further research is required to document what exactly is gained and what is lost by this replacement. If they provide different information, the two instruments could be used together in a complementary way.
To date, three studies have been published that evaluate the WHODAS 2.0 and GAF correlation in adult patients. The first evaluated 200 outpatients in Puerto Rico with any diagnosis and reported a positive, significant correlation of .37 between the scores of the two instruments (Martínez-Taboas et al., 2017). The second is a study conducted in the United States evaluating forty-two inpatients and outpatients with schizophrenia, which reported a significant, negative correlation of -.60 using an inverted GAF score. (Gspandl et al., 2018). The third is a Swedish study evaluating 522 patients with any diagnosis, which reported a significant, negative correlation of -.41 (Ramklint et al., 2022). To date, there have been no reports of these correlations in pediatric samples.
Evidence exists that some sociodemographic and clinical variables have been associated with low general functioning and global disability. These two aspects have been linked to lower levels of peer support (Chang et al., 2012), a greater number of comorbid internalizing and externalizing disorders (Dol et al., 2022), perinatal problems, such as preterm birth (Moster et al., 2008), and a history of emotional and sexual abuse (Mullen et al., 1996; Myroniuk et al., 2022). In this respect, it is necessary to evaluate the association between instruments such as the WHODAS 2.0 and GAF and the presence of such variables, particularly in pediatric samples.
We hypothesize that the correlation between WHODAS 2.0 and GAF scores would be low to moderate due to the high variability in severity and functioning evaluation in pediatric samples. Moreover, we consider that high comorbidity, and any kind of abuse would be significantly associated with low functioning in both instruments. The aim of this study was therefore to evaluate the correlation between the WHODAS 2.0 interview version (each domain as well as the total score) and GAF scores and to study the association between clinical and sociodemographic variables and functioning as assessed by the WHODAS 2.0 interview version and GAF in a psychiatric outpatient sample of children and adolescents in Latin America.
METHOD
Participants
The original sample was a convenience sample comprising outpatient children and adolescents (n = 74) referred for medical-psychiatric evaluation in any of the seven clinical sites (see below), from February to August 2016. The study included the subsample of patients who completed WHODAS 2.0 and GAF (n = 66).
Raters
Raters were the principal researchers of each clinical site with fifteen years’ experience and resident psychiatrists with at least four years’ experience in the assessment of pediatric patients. Each clinical site provided three to six different raters. All the raters were trained during a three-day theoretical-practical course when agreements were made in regard to the interview procedures for the K-SADS-PL, GAF and WHODAS 2.0; in the latter, any questions about sexual activity were omitted.
Study design and setting
All participant sites were clinical settings receiving either outpatients, inpatients, or both. The sites included two psychiatric hospitals, a university psychiatric outpatient service in Mexico City, a general hospital with psychiatric service in Aguascalientes, Mexico, a general hospital with psychiatric service in Medellin, Colombia, and two psychiatric hospitals in Santiago de Chile, Chile, and Montevideo, Uruguay.
Measurements
World Health Organization Disability Assessment Schedule (WHODAS) 2.0.
We used the full 36-item self-administered version of WHODAS 2.0, as included in the DSM-5. Studies have reported that the WHODAS 2.0 has high internal consistency (with a Cronbach’s alpha of .86), validity and reliability in epidemiological (Kimber et al., 2015) and clinical samples of young adolescents (Hu et al., 2012), and good concurrent validity with other instruments measuring a similar concept of disability (Hernández-Orduña et al., 2017). WHODAS 2.0 questions relate to the difficulties in functioning experienced by the interviewee during the previous thirty days. WHODAS 2.0 scores range from 36 to 180. Due to the low insight reported in psychotic patients (Hernández-Orduña et al., 2017), and the reading difficulties experienced by some children, as instructed by the DSM-5 clinician administration guide, the rater administered WHODAS 2.0 as an interview, simultaneously questioning the child/adolescent and parent/guardian and establishing a consensus answer.
Global Assessment of Functioning (GAF)
The GAF score (1 to 100) provides a classification of the subject’s psychological, social, and occupational functioning, ranging from positive mental health to severe psychopathology. The GAF has high internal consistency (with a Cronbach’s alpha of .74) (Söderberg et al., 2005). GAF values can be a single total score or range-type scores (Aas, 2011).
These instruments have opposite directions in their scores. Whereas a higher GAF score suggests higher functioning, a higher WHODAS 2.0 score indicates lower functioning. In this respect, a negative correlation would indicate that both scores correlate in their measure of functioning.
Clinical and psychosocial variables
We used the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS-PL-5), a semi-structured diagnostic interview designed to collect detailed sociodemographic and clinical information provided by the parent/guardian and child/adolescent to establish a diagnosis. Through the introductory interview of this instrument, we obtained the full psychosocial information provided by the K-SADS-PL-5, in other words, the participant’s status regarding parental divorce, complications at birth, abnormal development, maternal and parental history of mental illness, any kind of abuse and poor peer relationships. All these variables were coded dichotomously, as either present or absent. In the case of abuse, this was scored as present when any type (emotional, sexual, physical, or neglect) was present. Trained clinicians conducted the interview and used all responses to establish a more accurate clinical estimate for the symptoms in each disorder. The number of diagnoses was established after completing all the necessary appendices for each participant. Inter-rater reliability for all diagnoses included in the K-SADS-PL-5 ranged from moderate to good (kappa > .7; de la Peña et al., 2018a; de la Peña et al., 2018b).
Procedure
After receiving a thorough explanation of the research and after signing participation and assent/consent forms, the parent/guardian and the child/adolescent were interviewed for one to four sessions, lasting thirty to 120 minutes each. All participants were evaluated using the Spanish version of the K-SADS-PL-5. The WHODAS 2.0 and GAF were completed at the end of the interview.
Statistical analysis
Descriptive statistics are expressed as measures of means and standard deviation (SD) or frequency and percentages. A Spearman correlation between WHODAS 2.0 and GAF domains and total scores was calculated given the interval nature of the data. A general linear model analysis was performed to evaluate the association between selected sociodemographic and clinical variables with WHODAS 2.0 and GAF functioning scores. Analysis was performed using R (R Core Team, 2021). The level of significance was set at p < .05.
Ethical considerations
Informed assent and consent were obtained from all child/adolescent and parent/guardian participants in written form. Forms were signed after assenting/consenting to participate, with two witnesses also signing the same form. The authors declare that all procedures contributing to this study comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects/patients were approved by the Institutional Review Board of the INPRFM with authorization No. CEI/029/2020.
RESULTS
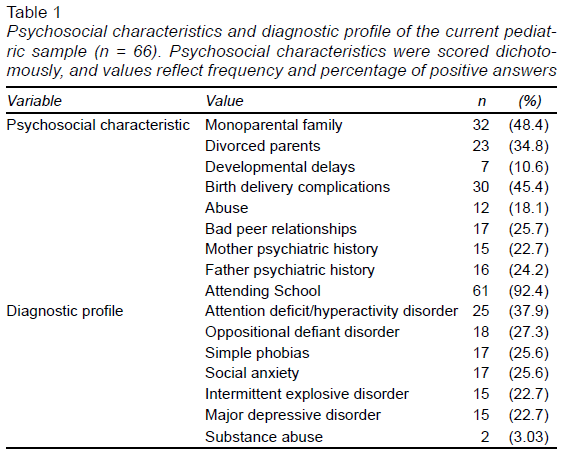
Sociodemographic and clinical characteristics are shown in Table 1. Most of the total sample (n = 66, 62.1% males, 11.4 years, SD = 3.2) were children actively attending school (92.4%). The mean number of diagnoses was 3.38 (SD = 2.78). More sample details can be reviewed in previous publications (de la Peña et al., 2018a; de la Peña et al., 2018b).
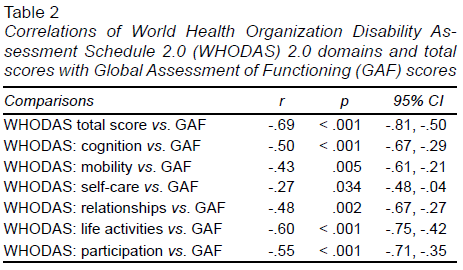
The mean WHODAS 2.0 and GAF scores were 60.48 (SD = 18.33) and 59.86 (SD = 17.10) respectively. WHODAS mean subdomains yielded the following scores: cognition = 11.38 (SD = 4.73), mobility = 6.41 (SD = 2.08), self-care = 5.12(SD = 1.72), relationships = 7.5 (SD = 3.01), life activities = 16.86 (SD = 7.68) and participation = 13.23 (SD = 5.36). The correlations between WHODAS 2.0 domains and total scores with GAF were all negative and significant (Table 2).
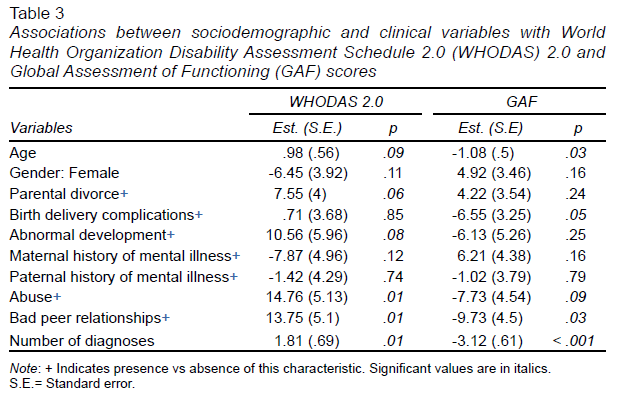
Regression analysis showed that although several variables contributed significantly to the variance of WHODAS 2.0 (R2 = .41) and GAF (R2 = .53), only the total number of diagnoses and poor peer relationship significantly contributed to the variance of both instruments (Table 3).
DISCUSSION AND CONCLUSION
We found negative and significant correlations between WHODAS 2.0 domains and total scores and GAF. Moreover, we found that only poor peer relationships and a higher number of diagnoses were associated with lower functioning scores on both instruments.
WHODAS 2.0 vs GAF
Some advantages and disadvantages have been described for both instruments. On the one hand, WHODAS 2.0 is completed during a semi-structured interview for any disease assessment of patient functioning in which impairment and disability are evaluated over six domains described during the past thirty days. It is reliable, responsive to change, and promoted by the WHO (Üstün et al., 2010; World Health Organization, 2010). Disadvantages include its limited familiarity due to its recent incorporation in the DSM-5, long application times (at least in the 36-item version) and the fact that it mainly uses activities that are meaningful for adults. On the other hand, GAF is completed by clinicians, used in a variety of settings, and has acceptable reliability when raters are experienced and trained (Gspandl et al., 2018). The disadvantages of GAF include the fact that it uses a single measure as an operationalization of more than one clinical phenomenon (psychological symptoms and social and occupational functioning). In addition, its validity diminishes when there is a discrepancy between symptom severity and functioning (Aas, 2011; Pedersen & Karterud, 2012). Finally, WHODAS subscales provide a detailed view of functionality, whereas GAF does not identify the specific domain that most affects the patient.
Previous studies of adult psychiatric samples have reported moderate to large significant correlations (Gspandl et al., 2018; Martínez-Taboas et al., 2017; Ramklint et al., 2022) between WHODAS 2.0 and GAF scores. In the current study, the moderate correlations could be explained by the fact that WHODAS 2.0 contains non-specific items, which most children or adolescents with psychopathology can perform without difficulty, such as those in the mobility and self-care domains. In our pediatric sample, these items were rated as “without problems,” leading to a better functioning score, whereas in the GAF evaluation, the clinician integrates functioning with psychiatric disorders, even though this is a controversial strategy (Smith et al., 2011). In view of this, we would recommend WHODAS 2.0 to evaluate psychiatric patients with a general medical condition that may include mobility, relationships, self-care, or participation disturbances that may not be present in all psychiatric patients. Interestingly, five out of the six domains in WHODAS 2.0 showed a moderate, significant correlation with GAF scores.
Although a WHODAS 2.0 version is available for children and adolescents, it is remarkably similar to the adult version (Scorza et al., 2013) but has not yet been incorporated into the DSM-5 or the DSM-5 revised version. The pediatric version requires further research before it can be widely used.
Functioning vs. sociodemographic and clinical variables
The results of the regression analyses confirmed previous reports regarding the association between sociodemographic and clinical variables and general functioning. In particular, poor peer relationships and a higher number of comorbid disorders were associated with low functioning in the scores of both instruments. In poor peer relationships, both instruments contain items that exclusively assess issues in this domain, which could explain the over-representation. Despite this, social relations in children and adolescents are one of the main pillars of the evaluation of functioning as was seen in the current sample. Children and adolescents spend a great deal of time with their peers who influence their behavior and values. Peer relationships serve as a bridge when adolescents move away from their parents towards independent adult functioning (Rohrbeck, 2003).
As for the number of diagnoses, a growing body of evidence about the commonality of triggers or factors associated with global psychopathology has led to a more dimensional approach to understanding mental illness. All psychopathological disorders are correlated not only at the disorder level, but also at the spectra level (Wright et al., 2013). Most common psychiatric disorders are therefore unified by a single psychopathology dimension, the p-factor (Caspi et al., 2014). Higher p-factor scores are associated with greater impairment in life and family dysfunction (Caspi & Moffitt, 2018). Previous studies have established that a higher number of diagnoses correlates with poor functioning (Caspi et al., 2014). If a higher number of diagnoses is associated with lower functioning, the dimensional diagnosis approach may need to be more frequently implemented. Variables such as complications at birth and having a history of abuse should be considered in future research to expand and achieve a better understanding of their impact on functioning outcomes.
Limitations
None of the participants in the sample were inpatients with severe disorders, which limits comparisons with other reports. The fact that this was a cross-sectional study meant that no association over time could be reported. The small sample size may have created a statistical bias. The way WHODAS 2.0 was applied limits its comparison with other self-report studies. Since global clinical severity was not evaluated, we were unable to use it as a covariate in the regression analysis.
Conclusion
The results of the current study provide evidence that WHODAS 2.0 and GAF scores appear to reflect similar aspects of functioning, as evidenced by the moderate correlation values. Poor peer relationships and a higher number of diagnoses are associated with lower functioning evaluations with WHODAS 2.0 and GAF. We therefore propose that in the case of younger patients, GAF could be used to complement WHODAS to obtain a full profile of the patient’s functioning, particularly in the self-care domain.