INTRODUCTION
The main purpose of primary health care (PHC) is to achieve the highest attainable level of health (World Health Organization [WHO], 2021). PHC includes comprehensive, integrated healthcare services focusing on primary care, public health policies; and the social participation of communities, families, and individuals in self-reliance and self-care for health (WHO, 2021).
In health care contexts, medication therapy adherence is a challenge in the clinical practice of health providers, including nursing professionals. WHO (2021) defines therapy adherence as the degree to which a person’s behavior, comprising medication intake, dietary follow-up, and lifestyle changes, corresponds to the recommendations of a health provider.
The literature shows how adherence can be associated with patient behavior regarding medicine intake by dosage, frequency, and medication regimen (Gast & Mathes, 2019). Medication nonadherence is associated with medication regimen complexity, lack of care continuity between the health provider and patient, fear of dependence or adverse effects (Ismail et al., 2017), psychological factors, educational attainment, and socioeconomic level (Gast & Mathes, 2019; Prakash et al., 2019).
The literature shows that there is a high percentage of patients who interrupt therapy without informing a health provider, and that approximately 50% of patients fail to take medication as prescribed (Kim et al., 2018). This scenario may reduce treatment efficacy, increasing the risk of recurrence of the pathology being treated (El Abdellati et al., 2020; Gupta et al., 2017) and encouraging the use of otherwise unnecessary and/or dangerously intensified therapies (Lam & Fresco, 2015), which can seriously harm patient health and possibly their quality of life (QoL).
The psychological barriers to adherence can be divided into two categories: intentional and unintentional (Martin et al., 2018). When intentional, the patient decides to modify or discontinue their treatment. When unintentional, the patient believes that the treatment is in fact being properly followed, or unintentionally fails to do so (such as forgetting to take the medicine at the correct time; Martin et al., 2018).
Psychotropic medications are a therapeutic class of medication that warrant highlighting when discussing medication adherence, given the complications resulting from inadequate use (El Abdellati et al., 2020). Patients with mental disorders have difficultly adhering to prescribed psychotropic medication, resulting in a high nonadherence rate among this population (Semahegn et al., 2020).
There is evidence that inadequate pharmacological treatment among people with mental disorders is more pronounced at PHCs than in specialized services, which is of particular interest to the present study. In addition, certain psychotropic medications are often prescribed for prolonged periods, contributing to treatment ineffectiveness and the likelihood of harm to the patient (Magin et al., 2018; Wand, 2019).
The literature notes that patients with common mental disorders (CMDs) are more likely to use psychotropic medication (Pereira Júnior et al., 2021). CMDs are a group of distress states manifesting as somatic symptoms, anxiety, and depression (Malhotra & Shah, 2015). A study of PHC patients observed that, compared with other patients, those with a CMD had lower QoL (Pereira Júnior et al., 2021). Furthermore, CMD patients using psychotropic medication have poor QoL (Miasso et al., 2017).
Other variables, such as clinical diseases, also significantly affect the QoL of the population served at PHC units (González-Blanch et al., 2018). It should be emphasized that QoL is a key indicator in relation to healthcare and global health needs and can be used as a basis for formulating public policies/recommendations.
Our study was designed based on the importance of PHC as a gateway to the health system, the high prevalence of CMDs, the importance and impact of medication therapy nonadherence, including psychotropic medications that have potentially serious consequences for patients, and the need to investigate the multiple factors potentially involved in medication therapy adherence and QoL.
In this study, we therefore sought to identify the predictors of nonadherence to psychotropic medication therapy and medication therapy in general, as well as quality-of-life predictors in medication users attending PHC units of the Unified Health System (UHS) in Brazil.
METHOD
Study design
This was a quantitative, observational, cross-sectional analytical study conducted of the UHS in Brazil at five PHC units in Ribeirão Preto, a municipality in the state of São Paulo, Brazil. We selected the PHC units with the largest catchment area in each health sector in the city under study.
Participants
A sampling plan was used to conduct stratified sampling with proportional allocation by strata. Each stratum comprised one of the five PHCs. The tolerable sampling error was 5%, and the level of significance 5%. A nonresponse rate of 15% was added, yielding a sample of 430 participants.
To collect the data, we approached participants waiting for medical appointments at the health units. Data were collected through individual interviews at the units under study. The inclusion criteria for the study were a) being aged 18 years or over and b) having a medical appointment scheduled in the units under study. The exclusion criterion was communication difficulties (such as impaired speech or hearing).
Measurements
Dependent variables
Dependent variables included adherence to psychotropic medication therapy, adherence to medication treatment in general, and QoL.
Independent variables and covariables
Independent variables were those associated with the sociodemographic profile (educational attainment, marital status, religion, occupation, number of family members), economic profile (monthly income, monthly family income), pharmacotherapeutic profile (medication use, psychotropic medication use, number of medications, number of pills taken daily, confidence in the doctor responsible for follow-up), and medical history (clinical diseases [self-reported] and common mental disorders). The covariables of sex and age were controlled for.
Procedure
Data for the independent variables and covariables were collected through a structured questionnaire created for the study, with questions on the respondent’s medical history and sociodemographic, economic, and pharmacotherapeutic profile.
We assessed medication adherence through the Measure Treatment Adherence-MTA (Delgado & Lima, 2001), a validated instrument comprising seven items for respondents to rate on an ordinal, six-point scale ranging from always (1) to never (6). The total MTA score was divided by the total number of questions, and the value was converted into a dichotomous scale. Values from one to four were considered to represent nonadherence while values from five to six were considered to represent therapy adherence. These procedures align with the recommendations available in the study validating the MTA (Delgado & Lima, 2001).
The validated Brazilian version of the Self-Reporting Questionnaire (SRQ–20), comprising 20 items (Mari & Williams, 1986) was used to track CMDs. Since cutoff points suggested by the validation study were used in this study, results were regarded as positive when female respondents answered “yes” to eight or more questions and male respondents answered “yes” to six or more questions.
We used the World Health Organization Quality-of-Life Assessment–BREF (WHOQOL–BREF; Fleck et al., 2000) to evaluate participants’ QoL. The Brazilian version of the WHOQOL–BREF was analyzed for the following psychometric characteristics: internal consistency, discriminant validity, concurrent validity, content validity, and test–retest reliability (Fleck et al., 2000). The WHOQOL–BREF comprises 26 questions encompassing four domains: (a) physical, (b) psychological, (c) social relations, and (d) environmental (The WHOQOL Group, 1998).
Statistical analyses
We analyzed the data using SAS (Version 9.2). Chi-square (χ2) tests were used to check the association between the dependent and independent variables. A logistic regression model was employed to measure the association between the variables of interest and nonadherence using odds ratio (ORs). We selected the variables for the adjusted model using the χ2 test result and chose the variables with a p value ≤ .20. This level of significance was adopted to identify the factors most closely related to nonadherence, not merely those with statistical significance, allowing for the inclusion of a greater number of variables in the logistic regression model. We only included variables without multicollinearity problems in the logistic regression model.
To compare the adherence groups and control for the effect of covariates on the WHOQOL–BREF scores, we conducted an analysis of covariance (ANCOVA).
We verified the reliability of the MTA using Cronbach’s α. For the adherence to medication in general variables, the coefficient found was .81 and a value of .91 was obtained for the adherence to psychotropic medication variable.
Because it is a dichotomous instrument, we measured the reliability of the SRQ–20 using the Kuder–Richarson coefficient (KR–20), which was equivalent to .85, showing good internal consistency.
In regard to the WHOQOL–BREF, we used Cronbach’s α. In this case, the coefficient was calculated for each domain, because each one consists of a subscale. The Cronbach’s αs for each domain were as follows: physical = .80, psychological = .75, social relations = .69, environmental = .74.
Ethical considerations
This study was approved by the Research Ethics Committee (Protocol No. 1474/2011) and followed the guidelines of the Brazilian National Research Council.
RESULTS
A total of 430 users from five PHC units in Ribeirão Preto, São Paulo, Brazil participated in the study. The sample consisted of people aged 18 to 83 (M = 45; range = 18–83, SD = 16.3). In the sample studied, the prevalence of CMD was 41.4%. In regard to pharmacotherapy, 65.6% of the participants used medication, while 25.8% of the total sample had been prescribed at least one psychotropic medication.
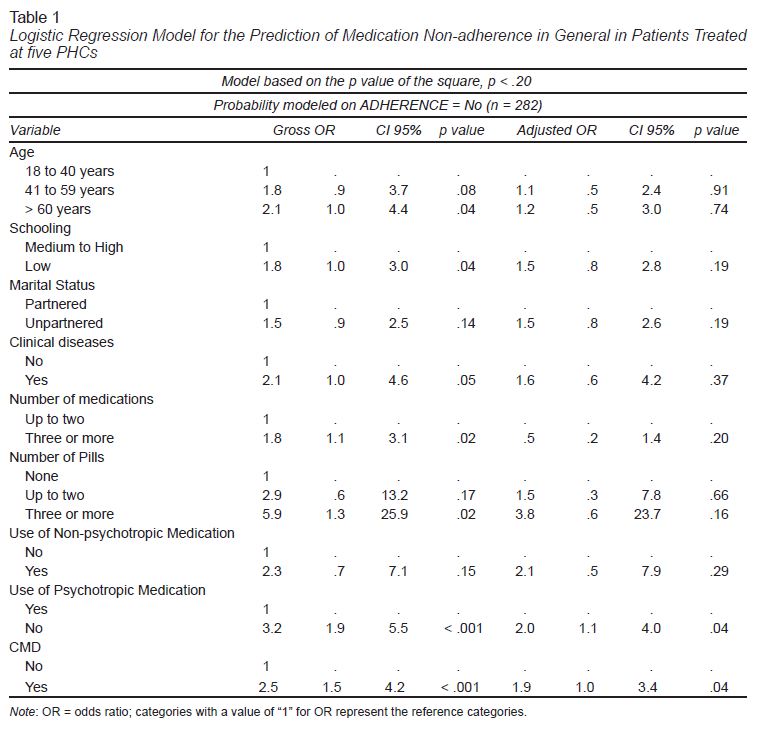
We developed a logistic regression model to evaluate predictors of nonadherence to medication in general. In the adjusted OR analysis, the CMD variables and the use of psychotropic medications were predictive of nonadherence to medication in general. Use of psychotropic medications was the strongest predictor of nonadherence, OR = 2.0 (p = .04, confidence interval [CI] [1.1, 4.0]), followed by CMD, OR = 1.9 (p = .04, CI [1.0, 3.4]). Participants using psychotropic medications were twice as likely not to adhere to prescription medications as those who did not use psychotropic medication, while participants with a CMD were twice as likely not to adhere to prescribed medications as those without a CMD.
Commonly, the most prescribed class of psychotropic medications was antidepressants (73%), followed by benzodiazepine anxiolytics (46.8%). Most prescriptions for psychotropic medications were written by general practitioners in the PHC network (56%), with only 17% being written by psychiatrists.
It worth noting that 42.3% of the participants were considered nonadherent to psychotropic medications.
We developed a logistic regression model to evaluate predictors of nonadherence to psychotropic medications. The gender and monthly income variables, and the question on confidence in the doctor responsible for the follow-up of the interviewees were part of the model. We observed that none of the variables significantly contributed to the model (Table 1).
Regarding QoL, we found that people who adhered to medications in general had higher QoL scores in all WHOQOL–BREF domains.
We created ANCOVA models to predict QoL scores in each domain. Given the objectives of the study and the literature on QoL, we included the following variables: CMDs, clinical diseases, use of psychotropic medication, sex, age, educational attainment, income, occupation, marital status, and medication adherence.
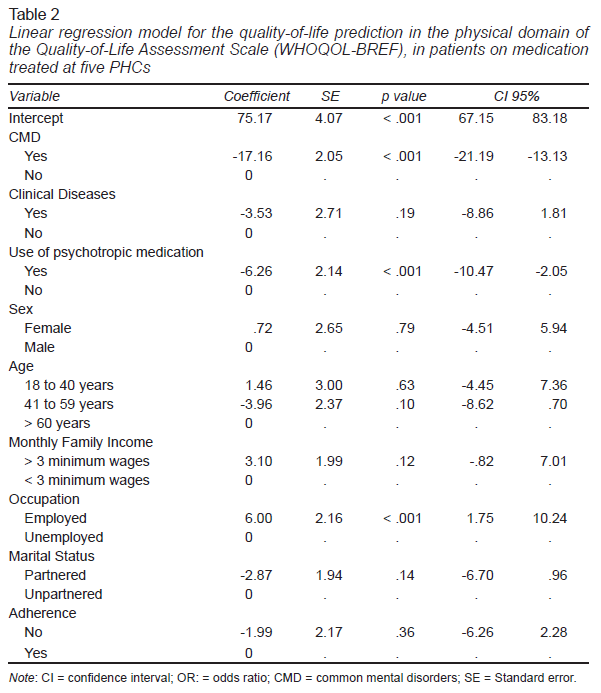
In the linear regression model for the physical domain, the predictors making a significant contribution to the model were CMD (p < .001), psychotropic medication use (p < .001), and occupation (p < .001). People with a CMD, and those who used psychotropic medications tended to obtain worse QoL evaluations, while those who were employed tended to have better QoL evaluations (Table 2).
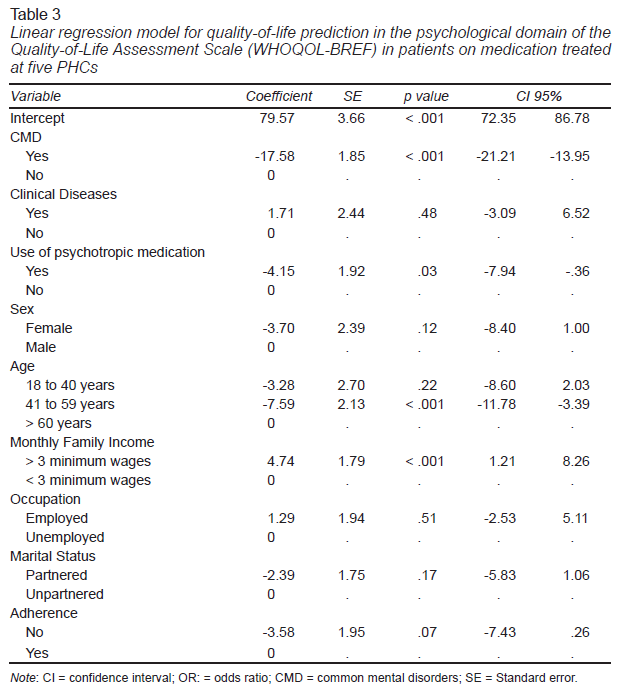
In the psychological domain, the predictors for worse QoL were as follows: having a CMD (p < .001), using psychotropic medications (p = .03), and being aged between 41 and 59 years (p < .001). Having an income of more than three minimum wages was predictor of better QoL (p < .001; Table 3).
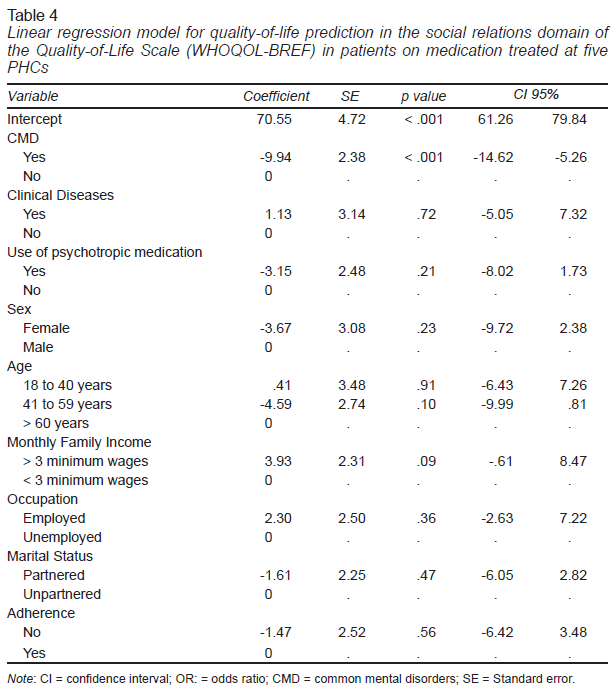
In the social relations domain, the CMD variable alone contributed significantly to the model (p < .001; Table 4).
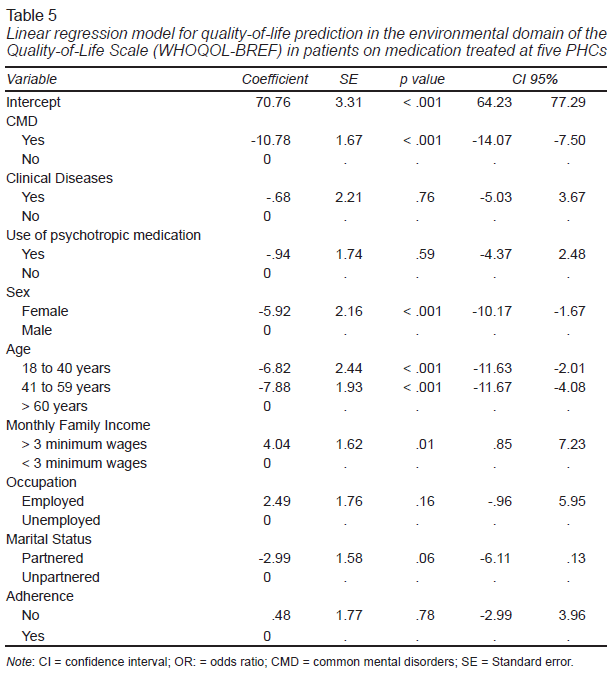
Regarding the environmental domain, the presence of a CMD was also one of the predictors of worse QoL (p < .001). Sociodemographic factors exerted a greater influence. In this case, the predictors found were sex (p < .001), income (p < .001), and age (p < .001). The age variable was significant in the following two categories: a) from 18 to 40 years and b) from 41 to 59 years. We found that belonging to the 18 to 40 and 41 to59 age groups, being female, and earning less than three minimum wages increased the chances of having worse QoL in the environment domain (Table 5).
DISCUSSION AND CONCLUSION
We found that 28% of the participants were considered nonadherent to medications in general. Although this percentage of nonadherence is not among the highest levels found, it impacts both patients and their families because it is associated with poor health outcomes. It also affects the healthcare system, because it results in higher costs (Jin et al., 2016; Miasso et al., 2016).
In the logistic regression model, in the adjusted analysis, CMD variables and the use of psychotropic medications were predictive of nonadherence to medications in general, while the use of psychotropic medications was the strongest predictor of nonadherence. There was a higher frequency of nonadherence among participants with a CMD. The literature confirms the negative influence of CMD on medication therapy adherence (Semahegn et al., 2020). In keeping with the existing literature, our findings raise the issue of the urgent need for actions targeting patients with symptoms of mental health conditions, because nonadherence can interfere with or impair treatment outcomes.
Furthermore, we identified worse QoL in individuals with a prescription for psychotropic medications. In fact, psychotropic medications for CMDs have been described as controversial in the literature. Their lower efficacy, and patients’ doubts about therapy efficacy can contribute to nonadherence to psychotropic medication (Semahegn et al., 2020). Psychosocial interventions focusing on pharmacological treatment could therefore be a promising strategy.
In our study, the psychotropic medications most often prescribed to patients at PHC units were antidepressants and benzodiazepines. Prescriptions for antidepressants have seen a steady increase in several countries (Brody & Gu, 2020; Estrela et al., 2020). Factors that can influence the increase of antidepressant prescriptions include a higher prevalence of CMDs, growing access to antidepressants and low investment in nonpharmacological therapies (Estrela et al., 2020).
Benzodiazepines are commonly prescribed to treat anxiety disorders (Tanguay Bernard et al., 2018). Some countries, such as Portugal (Estrela et al., 2020) and Canada (Tanguay Bernard et al., 2018), are concerned about chronic use of benzodiazepines. This concern is associated with long-term prescriptions, resulting in the risk of developing tolerance and dependence (Ogawa, 2019). Another important factor is when mental disorders are masked by somatic complaints (Zheng et al., 2019), making it difficult for clinicians unfamiliar with the cases to make an accurate diagnosis, resulting in the potentially indiscriminate prescription of psychotropic medications.
In our study, the rate of nonadherence to psychotropic medications was 42.3%, while the literature presents wide variations from approximately 20% to 81% (El Abdellati et al., 2020). The consequences of nonadherence to psychotropic medications can be serious, sometimes exacerbating the condition and possibly leading to rehospitalization (Semahegn et al., 2018). In addition to compromising the individual’s QoL and affecting cognitive, work, and social aspects, these consequences place a heavy burden on the family and entail high costs for the healthcare system (Semahegn et al., 2018).
Regarding medication adherence, there is evidence that behavioral and multifaceted interventions are more effective in promoting adherence to antidepressants than single component interventions (Pino-Sedeño et al., 2019). It should be emphasized that although, as a member of the health care team, the nurse is responsible for assisting the individual with their medication therapy, in our research, nearly all the information obtained by the participants on psychotropic medications was provided exclusively by physicians (98.4%).
We observed that health education is an important nursing intervention that was not in evidence in the health services under study. Among other aspects, this finding may reflect the lack of therapeutic listening, which allows people’s difficulties concerning medication treatment to be identified to select and guide individualized interventions.
In relation to QoL, adherent respondents obtained higher QoL scores in all domains of the WHOQOL–BREF. However, medication therapy adherence was not a predictor of better QoL in the multivariate analysis. About sociodemographic variables, the influences on QoL were statistically significant in the physical and environmental domains. We found that being unemployed was associated with worse QoL in the physical domain. This finding is supported by the literature (Tavakoli-Fard et al., 2016).
The environmental domain had the highest number of sociodemographic variables associated with QoL: age, sex, and income. We found that being aged 18 to 40 or 41 to 59, being female, and having an income of less than three minimum wages increased the chances of a worse QoL in the Environmental domain.
In relation to age, the literature has indicated worse QoL among older people because of the presence of chronic diseases (Ferretti et al., 2018; González-Blanch et al., 2018) and the presence of cognitive decline, affecting their performance of daily activities. This may also be associated with emotional changes and pain (Soósová, 2016), among other factors.
Regarding gender, other studies corroborate our findings in stating that men tend to rate their QoL higher than women do (Lee et al., 2020). The factors influencing adult men’s QoL can vary between studies and countries, the main factors being income, the environment, and physical and cognitive function (Bielderman et al., 2015; Lee et al., 2020).
The income variable is related to the environmental domain, because one of the issues comprising this aspect of QoL is financial resources. The literature corroborates the results of our research, noting that income is a key determinant of QoL in men and women (Lee et al., 2020). A good financial situation is therefore associated with better QoL. Another important point is that the stress created by a person’s current financial situation may have a greater impact on current mental health than previous life events (Barros et al., 2018).
In our study, having a CMD was the strongest predictor of worse QoL across all domains and the only factor associated with worse QoL in the social relations domain. Other studies have reported that CMD was a predictor of worse QoL (Ausín et al., 2020; Caron et al., 2019). Studies on the subject have shown that although CMDs can be spontaneously resolved, patients with a CMD continue to have a low QoL, corroborating the suggestion that CMDs cause functional impairment in patients and overburden health care systems (Kroenke et al., 2013).
Another relevant finding of our study is the identification of psychotropic medication use as a predictor of worse QoL in the physical and psychological domains. This result confirms the previously discussed hypothesis that, in this sample, psychotropic medications appear to have been used inefficiently. It is worth noting that one study has corroborated the findings of our study by observing that psychotropic medication users have worse QoL, report more somatic diseases, and have a greater need for medical care, together with a higher body mass index (Kopp et al., 2011).
Although psychotropic medications have many benefits, and are essential provided they are properly used, a possible explanation for their negative influence on QoL could be the wide range of their side effects (Semahegn et al., 2020). It is therefore important to advance the development of treatment guidelines to include multidimensional strategies to be implemented in PHC units to promote well-being and improve people’s QoL.
The results of our study should be interpreted considering its limitations. The first concerns its cross-sectional nature, which prevents the prediction of causality of the issues addressed. Another limitation is the use of a self-report instrument to assess medication therapy adherence, which may have prompted an overestimation of adherence.
The present findings indicate that strategies to promote medication therapy adherence in PHC services are necessary, especially among psychotropic medication users and people with a CMD.
People with a CMD are one of the largest groups attending PHC units. This is relevant, since this study found that they suffer from psychological distress, use more psychotropic medication than people who do not have a CMD and are therefore more susceptible to the side effects of these medications, and medication therapy nonadherence, all of which negatively affect their QoL.