INTRODUCTION
Pregnancy is a crucial period for a child’s physiological and psychological development. Maternal risk behaviors during this phase therefore have a significant impact on newborn health. Alcohol and tobacco consumption during pregnancy is a major public health concern because of its potential to harm maternal health, and fetal and embryonic development, and negatively impact child health (Scott & Sher, 2023).
Despite well-documented evidence of the teratogenic effects of alcohol and tobacco use during pregnancy, a sizable proportion of pregnant women continue to engage in these behaviors. Prevalence estimates of alcohol and tobacco use during pregnancy are broad and vary significantly by region. Globally, the prevalence of alcohol use during pregnancy is 9.8% (Popova et al., 2017), while tobacco use is 1.7%, amounting to 5.9% in the Americas (Lange et al., 2018). In Brazil, the prevalence of alcohol use during pregnancy ranges from 7.2% to 14% (Cabral et al., 2023; Dias et al., 2024; Pavesi et al., 2023). The prevalence of tobacco use during pregnancy ranges from 6.3% to 9.3% (Negrão et al., 2020; Pavesi et al., 2023). Given the significant prevalence and outcomes of the separate use of alcohol and tobacco during pregnancy, studies are required to examine the prevalence of the concomitant use of these substances and associated factors. However, studies evaluating the simultaneous use of alcohol and tobacco in pregnant women are scarce. Additionally, the available studies were conducted before the COVID-19 pandemic, which altered alcohol and tobacco use patterns in the population.
The scientific literature indicates that a complex set of factors are associated with alcohol and tobacco use during pregnancy, including mental health problems, obstetric variables, and sociodemographic and environmental characteristics (Dias et al., 2024; Kar et al., 2021). The analysis of socioeconomic contexts and access to health and obstetric services associated with substance use during pregnancy is essential given that this behavior constitutes a significant social problem. A study based on the analysis of medical records showed that factors such as inequality were associated with multiparous women and an insufficient number of prenatal consultations. In addition, smoking was correlated with lower education levels (Crisóstomo et al., 2022). Although some associations have been well established, other require further investigation. Research is needed to examine the factors linked to both individual and combined use of alcohol and tobacco during pregnancy, as this area remains insufficiently understood within scientific literature.
This study aimed to determine the prevalence of the separate and concomitant use of alcohol and tobacco during pregnancy and the associated sociodemographic, obstetric, and clinical factors.
METHOD
Study design
This is a cross-sectional, inferential study with a quantitative approach, based on the recommendations of the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) protocol.
Participants
The research was conducted at a public maternity hospital in the municipality of Rio Verde, in the southwest micro-region of the state of Goiás, in the west central region of Brazil. Participants were recruited using convenience sampling between February and April 2022. Postpartum women aged ≥ 18 years, whose pregnancies resulted in live births at the time of sample recruitment, conducted shortly after delivery and before hospital discharge, were included.
Because this was a study with convenience sampling from a finite population, a sample power calculation was performed. The sample power calculation for a bivariate logistic regression with 253 participants, a significance level of .05, an odds ratio of 1.5, and an event proportion of .3, yielded a sample power of approximately .864 (86.4%).
Measurement
The separate and combined use of alcohol and tobacco were evaluated as dependent variables in the present study. Substance use was assessed using the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST), validated for the Brazilian context (Henrique et al., 2004). Specific modules for alcohol and tobacco were used, and the defining question for use was “In the past three months, how often have you used the mentioned substance(s)?” Guidelines recommend that pregnant women abstain from consuming any alcohol or tobacco, as these are teratogenic substances and there is no consensus on safe consumption levels. Accordingly, responses other than “never” were categorized as substance use during pregnancy (Carson et al., 2010; World Health Organization [WHO], 2014; 2021).
The independent variables analyzed assessed the sociodemographic, obstetric, and clinical characteristics of participants. The questions covered age, skin color, educational attainment, marital status, family income, employment status, prenatal care, history of abortion, number of pregnancies, pregnancy complications, type of delivery, and start of prenatal care. Obstetric variables were evaluated by identifying the start and completion of prenatal care, number of pregnancies, pregnancy complications, type of delivery, number of live births, and history of previous abortion. The primary clinical variable assessed was the self-reported history of depression diagnosis, determined by asking participants whether they had ever received a diagnosis of depression from a healthcare professional.
Procedure
Postpartum women were recruited before hospital discharge, during which time the research objectives were presented. Those who agreed to participate received a link to access the questionnaire through their cell phones. Data were collected between the second and fifth days postpartum, following the recommendations of the Checklist for Reporting Results of Internet E-Surveys (CHERRIES).
Statistical analyses
Data analyses were performed using the Statistical Package for the Social Sciences version 29. Chi-square or Fisher’s exact tests were used to determine the association between the independent variables and substance use in bivariate analyses.
A multivariate logistic regression analysis was performed to assess the influence of independent variables on alcohol and tobacco use during pregnancy. Age was added to the regression models to control for confounding factors. Other variables included in the regression models were selected after significant association analysis in the bivariate analyses. The entry method was used to include independent variables in the models. The assumptions of multivariate logistic regression were verified using the Variance Inflation Factor (VIF) and Tolerance tests. Test results were acceptable, with VIF coefficients below 1.05 and tolerance below .98.
Ethical considerations
This study was conducted in accordance with the guidelines of the Declaration of Helsinki, particularly regarding informed consent. Additionally, ethical precepts established by Resolution 466/2012 of the Brazilian National Health Council were followed. All participants signed an Informed Consent Form (ICF) before beginning the study. The study was approved by the Research Ethics Committee (opinion number: 4.380.084).
RESULTS
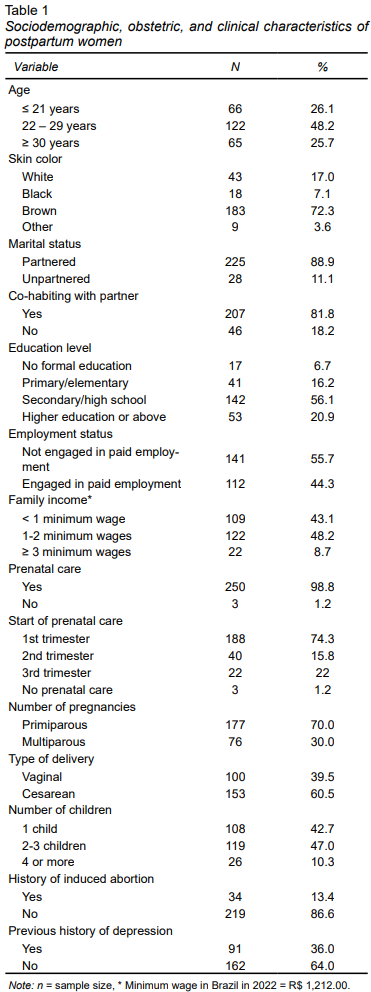
The sample for this study included 253 postpartum women, mainly within the age range of 22 to 29 years (48.2%), and with brown skin (83%). The majority of participants were partnered (88.9%) and living with their partners (88.9%). Regarding education, 56.1% had completed high school, 55.7% were unemployed, and 48.2% had a family income of between one and two minimum wages. Most patients had received prenatal care (98.8%) from the first trimester of pregnancy (74.3%). Most postpartum women were primiparous (70%) and did not experience complications during pregnancy (79.1%). Regarding the type of delivery, 60.5% had a cesarean section and 47% had two or three children. Regarding abortions, 13.4% reported a previous abortion, while 36% reported a depression diagnosis (Table 1).
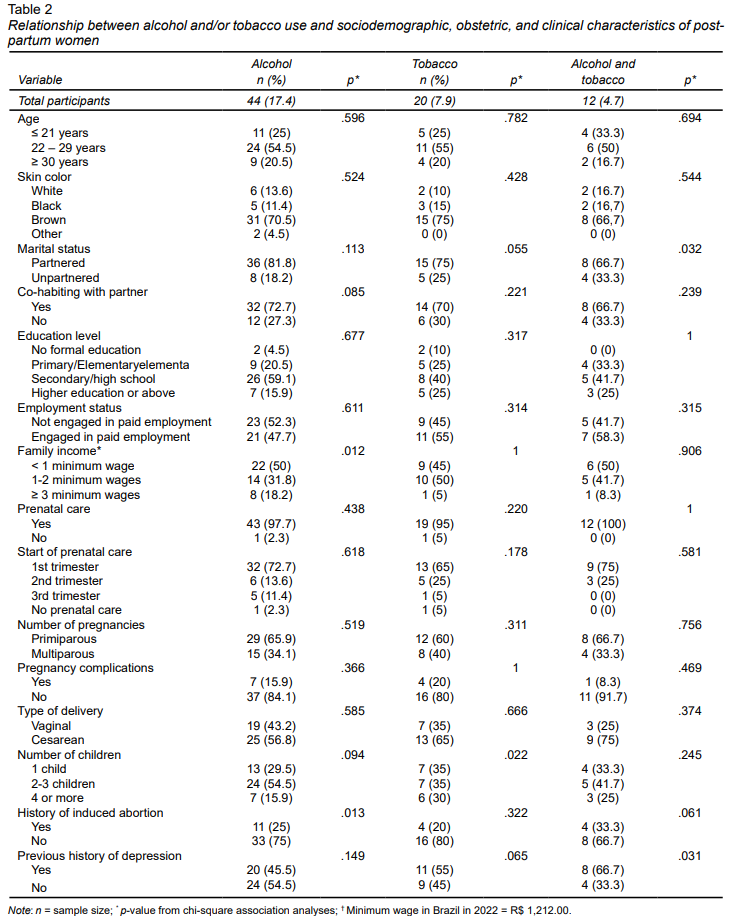
The results showed a prevalence of alcohol use of 17.4% (95% CI 13 - 22.1), tobacco use of 7.9% (95% CI 4.7 - 11.5), and combined alcohol and tobacco use of 4.7% (95% CI 2.4 - 7.5) during pregnancy. Table 2 presents the chi-square association analyses regarding the use of these substances with the sociodemographic, obstetric, and clinical variables of the postpartum women. An association was found between alcohol use and family income (p = .012) and previous abortions (p = .013). There was an association between tobacco use and number of children (p = .022). Combined use of these substances was linked to marital status (p = .032) and prior depression history (p = .031) (Table 2).
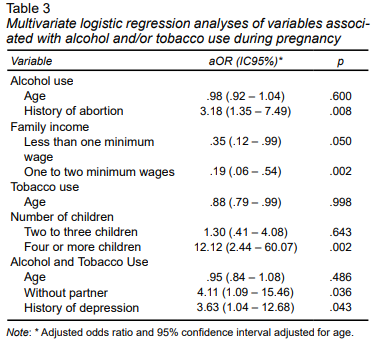
In the multivariate analyses, alcohol use was significantly associated with a history of induced abortion after controlling for age. Women who reported a previous abortion were 3.18 times as likely to use alcohol during pregnancy (Adjusted Odds Ratio [aOR] = 3.18; 95% CI: 1.35 - 7.49; p = .008). Regarding family income, those with an income below one minimum wage (aOR = .35; 95% CI: .12 - .99; p = .050) or between one and two minimum wages (aOR = .19; 95% CI: .06 - .54; p = .002) had a lower probability of alcohol use than women with a family income of three minimum wages or more. Tobacco use was significantly associated with a woman’s parity. Women who had four or more children were 12.12 times as likely to use tobacco than women with one child (aOR = 12.12; 95% CI: 2.44 - 60.07; p = .002). Unpartnered women were 4.11 times as likely to use both substances (aOR = 4.11; 95% CI: 1.09 - 15.46; p = .036). Moreover, those with a history of depression were 3.63 times as likely to combine alcohol and tobacco use (aOR = 3.63; 95% CI: 1.04 - 12.68; p = .043) (Table 3).
DISCUSSION AND CONCLUSIONS
In the present study, the prevalence of alcohol, tobacco, and combined alcohol and tobacco use during pregnancy was 17.4%, 7.9%, and 4.7%, respectively. The results also demonstrated associations between alcohol use and a history of induced abortion and family income, tobacco use and number of children, and combined alcohol and tobacco use and marital status and history of depression.
Studies have shown that the prevalence of alcohol and tobacco use during pregnancy varies according to the context in which the woman is admitted, the data collection method, and the instruments used. A study conducted in southern Brazil among low-risk pregnant women, utilizing the same assessment instrument as the current research and employing face-to-face interviews at Family Health Units, reported a prevalence of 14% for alcohol consumption and 28.5% for tobacco use (Dias et al., 2024). In the state of Santa Catarina, a study conducted of postpartum women found a prevalence of 7.2% for alcohol use and 9.3% for tobacco use (Pavesi et al., 2023). The prevalence of alcohol use in the present study (17.4%) was higher than that found in previous studies (14% and 7.2%) and lower (7.9%) in regard to tobacco use (28.5% and 9.3%). The combined use of alcohol and tobacco has not been widely explored in recent publications. However, a study conducted between 2011 and 2012 observed a prevalence of 2.2% among pregnant women (Cabral et al., 2023). This value is lower than that found in the present study, which recorded a prevalence of 4.7% among the postpartum women evaluated.
The discrepancies among study estimates should be interpreted cautiously, due to the inconsistent terminology utilized for alcohol and tobacco use during pregnancy, as well as the absence of standardized recommendations for assessment instruments (Cabral et al., 2023; Chagas et al., 2021). However, it is worth noting that most studies define substance use as any amount of consumption reported during pregnancy (Cabral et al., 2023; Dias et al., 2024; Pavesi et al., 2023). Furthermore, the guidelines for monitoring pregnant women, established by health agencies, recommend abstaining from alcohol and tobacco use during pregnancy, given the adverse consequences of use, even in small quantities (Ministério da Saúde, 2022; WHO, 2013).
Alcohol and tobacco use during pregnancy is associated with individual/subjective issues, sociocultural and environmental contexts, and a lack of information on the adverse consequences and the absence of technical approaches to the subject during prenatal care (Martinelli et al., 2021). Health professionals should implement effective strategies for screening for alcohol and tobacco use during pregnancy, considering modifiable factors that can be addressed by the health system, as recommended by the WHO (2014). Screening should be performed to ensure the timely identification of substance use and to increase pregnant women’s access to specialized mental health services, preferably with valid instruments such as the WHO ASSIST (Henrique et al., 2004).
It is important to note that, in this study, the assessment of alcohol and/or tobacco use specifically referred to the last trimester of pregnancy and that the timing of exposure to these substances can be influenced by a range of factors. Studies indicate that alcohol and tobacco consumption tends to decrease as pregnancy progresses, and is more prevalent in the first trimester (Tigka et al., 2023; Pereira et al., 2022). This reduction throughout pregnancy may be associated with increased awareness among women regarding the potentially negative consequences of using these substances for fetal development. It is therefore essential for preventive and educational actions to be implemented at the beginning of prenatal care, with the goal of early screening and intervention to help maintain reduced alcohol and tobacco use throughout pregnancy.
After pregnant women have screened positive for alcohol and/or tobacco use during pregnancy, health professionals should conduct brief interventions, to encourage them to continue to abstain from using these substances (Minozzi et al., 2024). Health professionals should implement a brief intervention strategy using evidence-based health education, to inform pregnant women of the adverse consequences of alcohol and tobacco use for the mother-child dyad. This intervention should be delivered with warmth and empathy to establish a bond with the pregnant women and reduce the stigma they face (Chang, 2020).
The present study promotes the identification and understanding of the factors entailing a higher risk of alcohol and tobacco use, to contribute to decision-making in actions designed to prevent the use of these substances during pregnancy. Alcohol consumption was associated with a history of previous abortion and family income.
As in the present study, research conducted in Ethiopia identified a 4.07-fold increase in the likelihood of alcohol use among women with a previous abortion (Bete et al., 2023). The relationship between a history of induced abortion and alcohol use during pregnancy can be explained by the fact that women who have experienced this situation may have high levels of stress and anxiety. They may resort to alcohol use as a coping strategy (Koly et al., 2023). It is therefore necessary to use practices designed to minimize the impact of this situation through low-density actions for primary health care. These include mindfulness practices, which have yielded satisfactory results as a coping strategy for mental health problems (Gherardi-Donato et al., 2023).
In the present study, women with a higher family income were at a higher risk of alcohol use. A study conducted with pregnant women in Japan showed that a higher family income was associated with an increased risk of alcohol use during early pregnancy, but not during mid-pregnancy (Murakami et al., 2020). In contrast to the results of the present study, research conducted in Brazil reported higher alcohol consumption among pregnant women with lower socioeconomic status (Cabral et al., 2023). Further studies should be conducted to evaluate the influence of income as a social determinant of alcohol consumption among pregnant women.
Research participants with more children were more likely to use tobacco during pregnancy. This association may stem from underestimating the risks of tobacco use during later pregnancies, particularly when prenatal counseling is lacking and pre-pregnancy tobacco habits persist (Odendaal et al. 2020).
Furthermore, postpartum women who were unpartnered or had a history of depression had a higher likelihood of combined alcohol and tobacco use during pregnancy. These results are in line with a previously published study by Bete et al., 2023. The authors suggest that the lack of social support, often obtained through an affective relationship, could explain the association between being unpartnered and combining alcohol and tobacco use. Finally, the association found between previous depression and substance use in the present study is corroborated by recent research findings that substance use may increase during pregnancy among women with a history of depression (Chapman et al., 2024).
Routine screening for alcohol and tobacco risk factors should be part of prenatal care, especially by nursing staff in primary health units. Professionals should be trained to provide psychosocial interventions and, if necessary, refer pregnant women to the Psychosocial Care Network to access specialized mental health services such as the Psychosocial Care Center for Alcohol and Drugs.
Identifying pregnant women who are more likely to use alcohol and/or tobacco during pregnancy is crucial to guiding interventions. However, the results of this study have certain limitations. Key variables for identifying factors associated with substance use, such as pregnancy planning and a history of induced abortion, were not evaluated. Online data collection may introduce sampling bias, as it may fail to capture the experiences of individuals without internet access or digital devices. Moreover, self-reported alcohol and tobacco use during pregnancy may be underestimated because of social desirability bias and stigma. In this study, we used confidential online assessments to minimize social desirability bias and obtain accurate responses from participants.
Alcohol and tobacco use during pregnancy is a public health issue requiring urgent attention from the health system. Research indicates that factors such as a history of induced abortion, family income, number of children, marital status, and prior experiences with depression each uniquely affect the likelihood of substance use during pregnancy.
Given the substantial impact of these substances on maternal and fetal health, it is essential to implement strategic, comprehensive programs designed to structure effective measures for the control and prevention of alcohol and tobacco consumption during the gestational period. Raising awareness among health professionals and creating targeted public policies are crucial steps towards promoting healthy pregnancies and ensuring the well-being of both mothers and babies.